Front Oncol:真实世界中CA199的监测模式跟转移性胰腺导管腺癌(PDAC)预后的关系
2021-10-23 yd2015 MedSci原创
真实世界数据表明,治疗前CA199的水平影响mPDAC的预后。治疗期间对CA199的监测有助于改善患者预后。今后需要进一步研究证实。
胰腺癌是一种致命的恶性肿瘤,在所有癌症中死亡率较高。它目前是美国癌症相关死亡的第三大原因,仅次于肺癌和结肠癌。胰腺导管腺癌(PDAC)是最常见的胰腺癌类型,约占85%的病例。所有诊断为PDAC的患者的5年相对生存率为10%,而转移性疾病患者的生存率低于3%。目前,血清碳水化合物抗原19-9 (CA 19-9)是美国食品和药物管理局(FDA)批准的唯一用于胰腺癌治疗的生物标志物。CA19 -9检测的灵敏度为80%,特异性为80-90%。近期,国外学者开展了相关研究,评估真实世界中CA199的监测与转移性胰腺导管癌(PDAC)的临床预后的关系。相关结果发表在Frontiers in Oncology杂志上。

收集2015年1月1日至2020年6月30日期间诊断为mPDAC的患者相关临床以及预后资料。同时收集基线时的血清CA 19-9水平(定义为治疗开始前60天)和治疗期间的水平值。CA 19-9 >40 IU/mL被认为是升高。根据检测频率、基线CA 19-9水平和CA 19-9变化比较生存结果。
在2015年1月1日至2020年6月30日期间,8776例患者被确诊为mPDAC。这些患者中约有四分之三(n=6,142)接受了1线全身治疗。6118例患者符合所有的研究选择标准。最终的研究分析根据CA199的检测模式分为四个独立的队列:无检测队列(n=781),仅基线检测队列(n=1082),在1线治疗期间进行一次检测队列(n=896),在1L治疗期间中进行多次检测队列(n=3,359)。
在纳入的6,118例mPDAC患者中,39.3% (n=2,402)的患者在2线治疗,12.9% (n=790)的患者在3线治疗。所有患者诊断的中位年龄为68岁(IQR: 61-75),55%为男性。总的来说,大多数患者(67.1%)是白人,而8.5%是黑人,1.8%是亚洲人,只有0.2%是西班牙人。在基线评估CA 19-9的患者中,大多数(84.7%)CA 19-9基线升高。
63%基线CA 19-9水平升高的患者接受了多次检测,而54%基线CA 19-9水平正常的患者接受了多次检测。与基线时CA 19-9水平正常的患者相比,治疗开始时CA 19-9水平升高的患者中位OS (mOS)更差。与基线时CA 19-9水平正常的患者相比,而基线CA 19-9水平升高的患者接受1线,2线和3线的mOS值都更差[1L: 8.8个月 (95% CI: 7.9 - 10) vs. 7.2个月 (6.8 – 7.5), p < 0.001; 2L: 7.2个月(6.1 – 9.2) vs. 5.2个月 (4.9 – 5.6), p < 0.001; 3L: 6.1个月(5.4 – 9.1) vs. 3.9 个月(3.4 – 4.3), p < 0.001]。
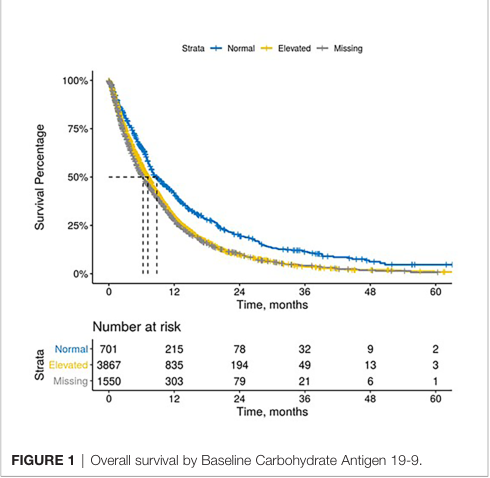
OS
此外,mPDAC患者进行CA 19-9多次测试的有更好的状态和更长的mOS。在治疗过程中接受CA 19-9多次评估的患者,ECOG PS评分为2+的患者比例最低。在治疗期间进行多次检测的患者比仅进行一次检测或仅在治疗前进行一次检测的患者mOS更长。
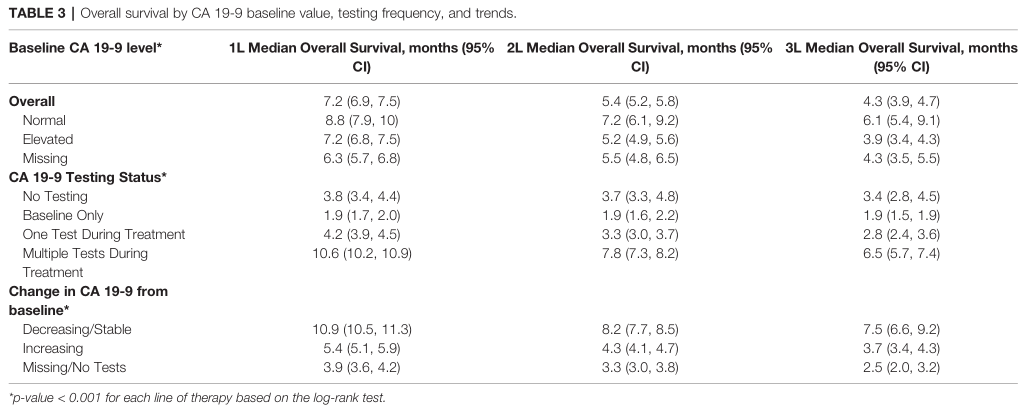
OS分层
在治疗期间相对于基线CA 19-9稳定和下降的患者比在治疗期间CA 19-9升高的患者mOS更好[1L: 10.9个月 (10.5 – 11.3) vs. 5.4 个月 (5.1 – 5.9), p < 0.0001; 2L: 8.2个月 (7.7 – 8.5) vs. 4.3个月 (4.1 – 4.7), p < 0.001; 3L: 7.5 个月 (6.6 – 9.2) vs. 3.7个月 (3.4 – 4.3), p < 0.001]。从基线增加CA 19-9水平与较短的中位OS相关,这些趋势在按治疗线分层时仍然存在。在1L治疗的患者中,降低最大的患者mOS最长。
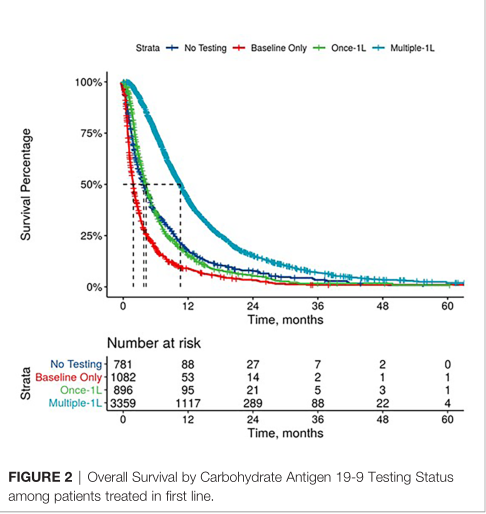
1线OS对比
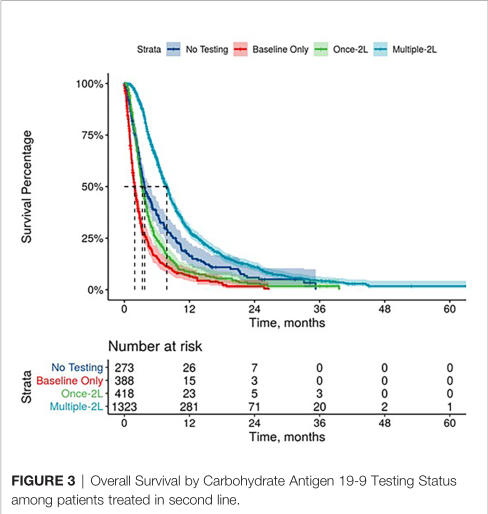
2线OS对比
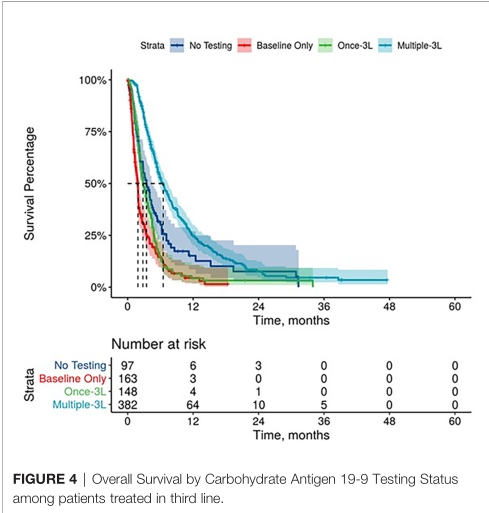
3线OS对比
综上,真实世界数据表明,治疗前CA199的水平影响mPDAC的预后。治疗期间对CA199的监测有助于改善患者预后。今后需要进一步研究证实。
原始出处:
George B, Kent M, Surinach A, Lamarre N and Cockrum P (2021) The Association of Real-World CA 19-9 Level Monitoring Patterns and Clinical Outcomes Among Patients With Metastatic Pancreatic Ductal Adenocarcinoma. Front. Oncol. 11:754687. doi: 10.3389/fonc.2021.754687
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Oncol#
25
#CA199#
26
学习了
37
#真实世界#
30
#转移性#
25
为胰腺癌病变诊断,带来了益处
58
不错
45