JCO:恩曲替尼治疗局部晚期或转移性ROS1融合阳性NSCLC总体安全有效,颅内ORR可达79.2%
2021-03-02 MedSci原创 MedSci原创
恩曲替尼在这些患者中总体疗效(ORR为67.1%,中位有效时间15.7个月)和颅内疗效(可测量基线的CNS转移患者的颅内ORR为72.9%)仍然很强,安全有效。
恩曲替尼在这些患者中总体疗效(ORR为67.1%,中位有效时间15.7个月)和颅内疗效(可测量基线的CNS转移患者的颅内ORR为72.9%)仍然很强,安全有效。

Journal of Clinical Oncology 昨日发布了恩曲替尼在ROS1融合阳性非小细胞肺癌(NSCLC)中的3个I期或II期临床试验(ALKA-372-001、STARTRK-1和STARTRK-2)的最新综合分析结果。
酪氨酸受体激酶ROS原癌基因1(ROS1)的基因重排是非小细胞肺癌(NSCLC)的致癌驱动因素。
因此,研究者有了新的思路,可否延长随访时间,在更大的人群中证实恩曲替尼在局部晚期或转移性ROS原癌基因1(ROS1)融合阳性非小细胞肺癌患者(包括基线时有中枢转移的患者)中的有效性和安全性?
为此研究纳入了患有局部晚期或转移性ROS1融合阳性NSCLC,伴或不伴有CNS转移的成年患者。这些每天口服恩曲替尼≥600毫克,在较长的随访时间中评估疗效。该研究设立客观应答率(ORR)为共同主要终点,并采用盲法独立中心评价和应答持续时间(DOR)。次要终点包括无进展生存期(PFS)、总生存期(OS)、颅内ORR、颅内DOR、颅内PFS和安全性。
在随访长于6个月、综合疗效评估人群中(n = 161),STARTRK-2入组145例,STARTRK-1入组7例,ALKA-372-001入组9例。中位治疗时间为10.7个月(IQR,6.4-17.7)。通过BICR评估,大多数患者的目标病灶变小,在108例患者(67.1%,95%CI,59.3-74.3)中实现了明确的客观缓解,有14例实现CR(8.7%)和94例获得PR(58.4%)。另有14名患者(8.7%)病情稳定。响应发生较早(响应的中位时间为0.95个月,范围为0.7-26.6个月)。
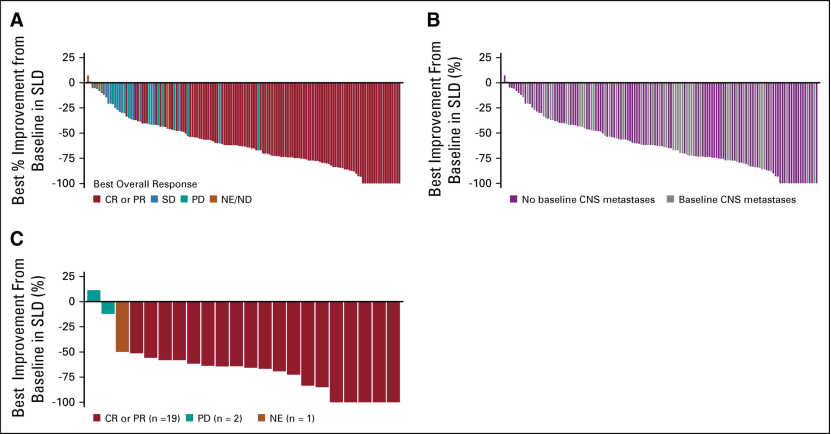
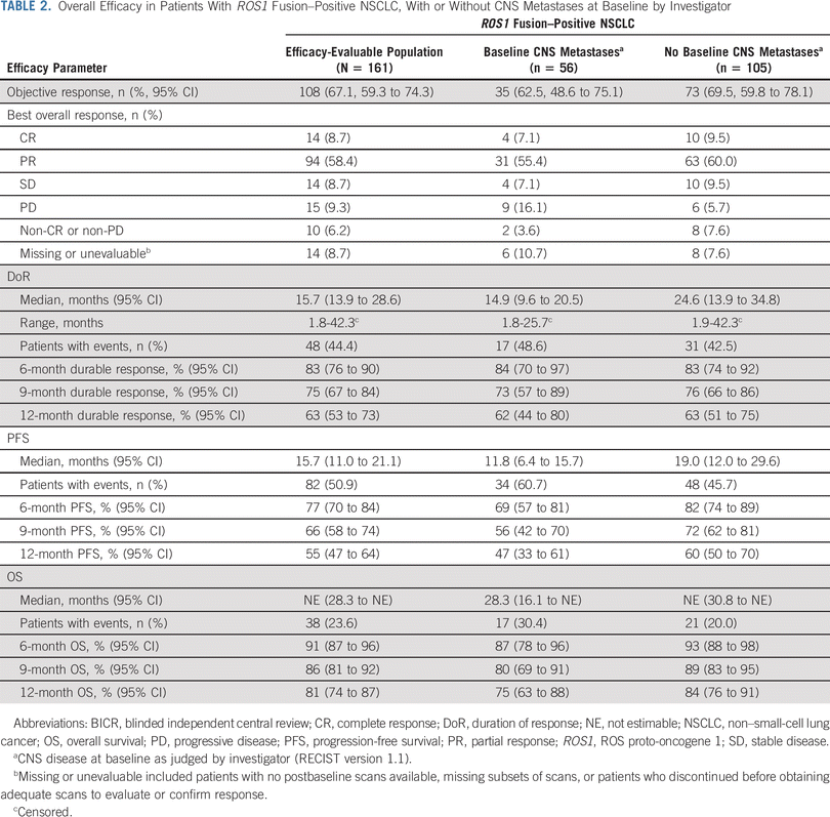
ORR为67.1%(n=108,95%CI 59.3-74.3),疗效持久(12个月DOR率63%,平均DOR 15.7个月)。12个月PFS率为55%(中位PFS为15.7个月)。
24例CNS转移患者的颅内ORR为79.2%(n=19,95%CI 57.9-92.9),中位PFS为12.0个月(95%CI 6.2-19.3),中位DOR为12.9个月(12个月率为55%)。研究者判断,不论基线时的CNS疾病状况如何,ORR都是一致的。具有CNS转移的患者的ORR为62.5%,而无CNS转移的患者的ORR为69.5%。几乎没有基线CNS转移的患者报告通过扫描证实了CNS进展(n = 3/105,2.9%),在基线CNS转移的56例患者中有27例(48.2%)有CNS进展。OS结果仍不成熟,12个月OS率为81%(中位OS为NE),38名(23.6%)患者在随访期间死亡。
在该研究分析中,恩替替尼的总体ORR(67.1%)与其他ROS1抑制剂的疗效相同。在ROS1融合阳性的TKI初治患者中,克唑替尼(72%,n = 38/53,PROFILE 1001;71.7%,n = 91/127,OxOnc),劳拉替尼(62%,n = 13/21)和赛瑞替尼(62%,n = 20/32)是一致的。但是,鉴于研究人群之间的固有差异,应谨慎考虑交叉试验的比较。

根据研究者评估,在基线时对中枢神经系统疾病患者的扫描结果进行了BICR扫描后,证实有46例患者中枢神经系统转移。其中有24例患有可测量的疾病。所有具有中枢神经系统基线转移(可测量或不可测量)的患者的颅内ORR为52.2%(n = 24; 95%CI,37.0至67.1),其中包括8例(17.4%)获得颅内CR。
在基线时可测量的CNS转移的24例患者中,颅内ORR为79.2%(n = 19,95%CI,57.9至92.9),其中3例(12.5%)获得颅内CR。在中枢神经系统转移灶可测量或不可测量的24名应答者中,颅内应答中位时间为0.95个月(范围0.7-6.4)。应答是持久的,12个月的颅内DoR率为55.0%。可测量或不可测量的中枢神经系统转移患者的颅内PFS中位数(95%CI)为8.3个月(6.4至15.7);31名患者(67.4%)经历了不良反应事件(疾病进展,n = 24;死亡,n = 7)。在可测量或不可测量的CNS转移患者中,颅内PFS维持至少12个月。在开始恩替替尼前至少6个月未接受脑放疗或接受脑放疗的患者中,颅内ORR为46.2%(95%CI,26.6至66.6)。
研究者认为,这项综合分析显示的颅内益处具有特殊的临床意义,因为其他可用的ros1抑制剂对颅内活性的有力证据是有限的(赛瑞替尼25%,n=2/8和劳拉替尼64%,n=7/11),而在基线时,高达40%的ros1融合阳性转移性非小细胞肺癌患者伴有中枢神经系统疾病。在恩曲替尼获得批准之前,对局部晚期或转移性ROS1融合阳性NSCLC患者的中枢神经系统活性治疗的需求尚未得到满足。除了证实恩曲替尼的总体疗效外,该研究结果强力证明恩曲替尼可以治疗现有的CNS转移,并可能具有潜在的CNS保护作用。

安全状况与之前的报告一致。未发现新的安全信号。几乎所有的TRAE均为1-2级,最常见的是味觉不良(n = 90,42.9%),头晕(n = 72,34.3%)和便秘(n = 66,31.4%)。大多数AEs是低等级的,可管理的,并可比于其他ROS1抑制剂。观察到恩替替尼停药的发生率较低,并且高剂量强度表明,任何剂量修改对总体暴露的影响均很小,大多数患者均接受了计划的全部剂量。
该研究的不足主要是样本量相对较小和单臂设计。此外,对于进行后的组织收集没有强制性要求,并且对恩替替尼的获得性耐药性的特征尚待鉴定。但可喜可贺的是,恩曲替尼继续显示出对ROS1融合阳性NSCLC患者的高度临床益处,尤其是伴有CNS转移的患者。
Reference:
Rafal Dziadziuszko, Matthew G. Krebs, Filippo De Braud, et al. Updated Integrated Analysis of the Efficacy and Safety of Entrectinib in Locally Advanced or Metastatic ROS1 Fusion–Positive Non–Small-Cell Lung Cancer. Journal of Clinical Oncology 0 0:0. Published online March 01, 2021.
DOI: 10.1200/JCO.20.03025
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#阳性NSCLC#
27
#局部晚期#
35
#JCO#
29
总体安全有效颅内ORR可达
68
#ROS#
26
#转移性#
24
#局部#
22
#融合#
26
#ROS1#
52
#ORR#
25