Radiology:这些CT表现,让急性胰腺炎达到“标本兼治”!
2022-01-12 shaosai MedSci原创
急性胰腺炎(AP)是十分常见的炎症性疾病,胆结石是诱发AP的主要因素之一。因此早期识别胆道病变是预防AP至关重要的手段之一,早期的诊断及干预可避免并发症的发生和疾病的复发。
急性胰腺炎(AP)是十分常见的炎症性疾病,胆结石是诱发AP的主要因素之一。因此早期识别胆道病变是预防AP至关重要的手段之一,早期的诊断及干预可避免并发症的发生和疾病的复发。在急性胆汁性胰腺炎(ABP)并发胆管炎和胆道梗阻时,建议早期进行内窥镜逆行胰胆管造影检查,否则将导致病情的延误及胆道并发症的发生。
严重程度分期是入院后AP管理的强制性步骤之一。腹部CT扫描由于可以显示急性胰腺水肿和坏死,因此仍然是临床进行病情严重程度评估的重要基石之一。但据我们所知,CT对明确病因的价值尚不明确
近日,发表在Radiology杂志的一项研究评估了与ABP相关的腹部CT影像学特征,并评估了CT征象和临床数据相结合的预测价值,为首次发作AP的病因确定提供了参考依据,实现了AP患者的早期治疗及预后的提高。
从2014年12月到2019年5月,本研究对所有首次出现AP并有至少6个月随访记录的患者进行了评估。胆结石是ABP临床诊断所必须的一项。腹部CT图像由两名腹部放射科医生进行审阅。进行了单变量和多变量统计分析,并在临床数据和CT特征的基础上构建了一个列线图,并在另一个独立的内部患者群中进行了验证。
共评估了271名患者(平均年龄±标准差,56岁±20岁;160名男性)。其中,170人(63%)有ABP。在多变量分析中,年龄(几率[OR],1.06;95% CI:1.03,1.09;P < .001)、丙氨酸转氨酶水平(OR,1.00;95% CI:1.00,1.01;P = .009)、胆囊胆石(OR,15.59;95% CI:4.61,68.62;P < . 001)、胆道环征(OR,5.73;95% CI:2.11,17.05;P < .001)、肝脏自发性衰减(OR,1.07;95% CI:1.04,1.11;P < .001)和十二指肠增厚(OR,0.17;95% CI:0.03,0.61;P = .01)都与ABP独立相关。结合临床数据和CT特征的匹配列线图在研究样本(n = 271)中显示出了0.94(95% CI: 0.91, 0.97)的曲线下面积,在验证队列(n = 51)中为0.91(95% CI: 0.84, 0.99)。
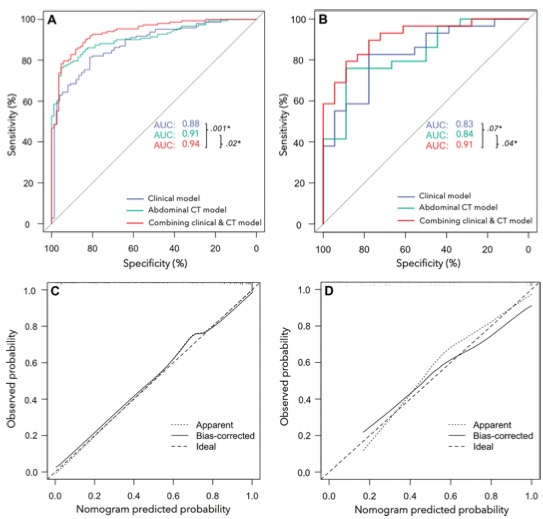
图 (A, B)研究样本(A)和验证队列(B)中诊断急性胆汁性胰腺炎(ABP)的临床模型、CT模型和联合模型的曲线下面积(AUC)。在研究样本和验证队列中,联合模型显示了预测ABP的最佳诊断性能(AUC,0.91[95% CI:0.818,0.986])。*=AUC与Delong测试的比较。(C, D)研究样本(C)和验证队列(D)中组合模型的校准曲线。
本研究表明,急性胰腺炎(AP)的部分早期腹部CT征象为诊断急性胆汁性胰腺炎(ABP)提供了十分有力的支持。CT表现和临床数据的结合表现出了对AP胆道因素的最佳诊断性能。由于ABP的早期诊断至关重要,因此本研究认为腹部CT应被纳入ABP早期诊断的一线检查手段。由于现阶段,CT更多的用于评估AP的严重程度,然而其对病因学诊断的贡献也不应该被忽视,这可减少患者不必要的检查并提高患者的治疗预后。
原文出处:
Thibaut Zver,Paul Calame,Stéphane Koch,et al.Early Prediction of Acute Biliary Pancreatitis Using Clinical and Abdominal CT Features.DOI:10.1148/radiol.2021210607
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#标本#
58
#胰腺炎#
78
#CT表现#
50
学习了
54
优秀的
63
非常感谢
55