Ann Oncol:帕妥珠单抗+曲妥珠单抗+紫杉类一线治疗HER2阳性局部复发或转移性乳腺癌的疗效和安全性:PERUSE研究的最终分析
2021-07-10 yd2015 MedSci原创
PERUSE研究的最终结果显示其安全性和有效性与CLEOPATRA研究类似,中位OS超过了5年。结果表明紫杉醇是一种有效的可替代多西他赛作为基础化疗药物。
在HER2阳性转移性乳腺癌中,来自随机III期临床研究CLEOPATRA的结果确立了帕妥珠单抗+曲妥珠单抗+多西紫杉醇一线治疗的新标准。与单一抗HER2治疗相比较,双重HER2阻断显著改善了患者的无进展生存期(PFS)和总生存期(OS)。PERUSE (NCT01572038)研究是一项全球多中心的单臂研究,评估帕妥珠单抗+曲妥珠单抗+三种常用紫杉醇类药物(多西他赛、紫杉醇和白蛋白紫杉醇)一线治疗HER2阳性局部复发或转移性乳腺癌((LR/mBC)的疗效和安全性。初期分析结果发现紫杉醇+帕妥珠单抗+曲妥珠单抗跟多西他赛联合组的疗效相近,但是毒性更少。目前,Annals of Oncology杂志更新了最终分析结果。
主要研究终点是安全性。次要研究终点包括无进展生存期(PFS)和总生存期(OS)。预先指定的亚组分析包括根据紫杉类药物、激素受体(HR)状态和既往曲妥珠单抗进行的分层。在1436例接受治疗的患者中,研究者最初选择的多西他赛有775例(54%),紫杉醇有588例(41%),白蛋白结合型紫杉醇有65例(5%)。中位随访时间为68.7个月(95% CI 67.5–69.3; range 0.0–87.3)。
最常见的不良事件(AEs)是胃肠道和皮肤/皮下事件。61%的患者发生了≥3 级不良事件,20%与帕妥珠单抗有关,17%与曲妥珠单抗有关,36%与紫杉类药物有关。最常见的≥3级不良事件是中性粒细胞减少(10%)和腹泻(8%)。多西他赛组出现更高的≥3级中性粒细胞减少发生率(15%对比5%和2%的病人接受紫杉醇和白蛋白结合型紫杉醇)和≥3级发热性中性粒细胞减少(11%对比1%,0%)。≥3级腹泻的发生率在三种紫杉类药物中相似(分别为8%、9%和8%)。31例(2%)患者报告了致命的不良事件。超过1例患者中报告的致命AE报告有肺炎(n = 4)、脓毒症(n = 3)和心脏骤停(n = 2)。10%的患者因不良事件导致停用帕妥珠单抗,9%的患者停用曲妥珠单抗,20%的患者停用紫杉烷。最常见的导致治疗停止的不良事件是射血分数下降(3%)和心力衰竭(0.7%),导致了停止帕妥珠单抗和曲妥珠单抗;而周围神经病变(4%),周围感觉神经病变(2%),感觉异常(2%),腹泻(1%),疲劳(1%),虚弱(0.9%)和甲骨溶解(0.6%)导致紫杉类药物的停药。

不良事件
总评估人群的客观缓解率(ORR)为79% (95% CI 77–82%)。临床获益率为86% (95% CI 84–88%)。中位治疗至应答时间为2.5个月(95% CI 2.4–2.5) ,中位持续应答时间为20.0个月(95% CI 18.2–22.2)。意向性人群(ITT)的中位无生存期(PFS)为20.7个月(95% CI 18.9 23.1)。亚组分析显示,无论HR 状态或紫杉类药物,无进展生存期相似,但对之前没有曲妥珠单抗的亚组有利。
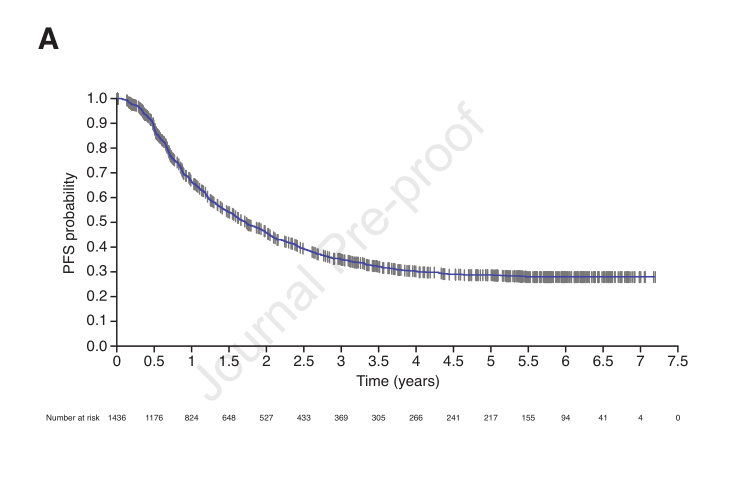
ITT PFS
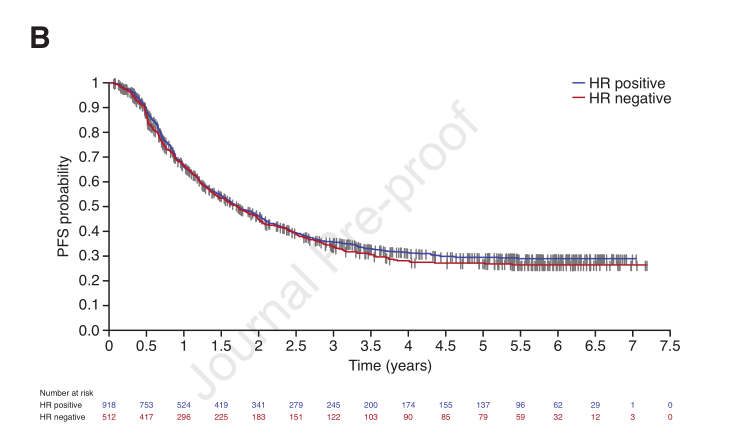
HR分组 PFS
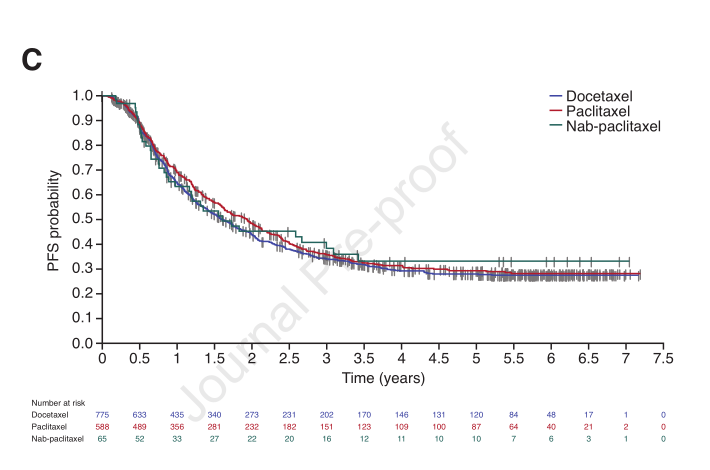
紫杉类药物分组PFS
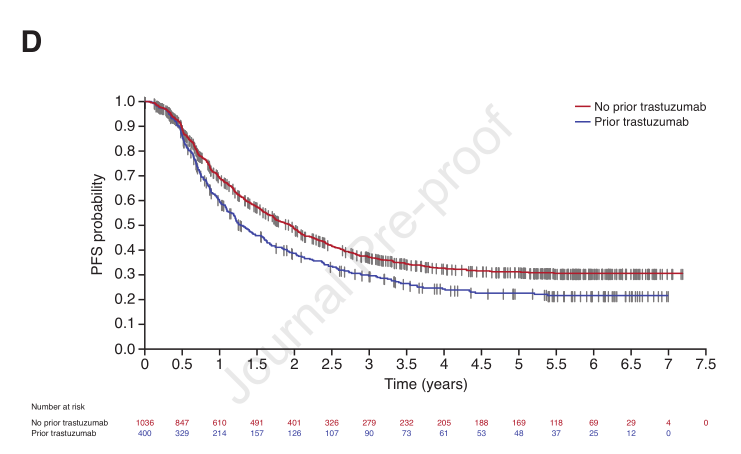
既往有无曲妥珠单抗PFS
ITT患者的中位OS为65.3个月(95% CI 60.9 70.9个月)。紫杉类药物亚组的OS相似,多西他赛和紫杉醇的Kaplan-Meier曲线重叠。然而,OS在HR阳性患者中比HR阴性患者中更有利,在既往无曲妥珠单抗患者中比既往有曲妥珠单抗患者中更有利。

ITT OS

HR分组 OS

紫杉类药物分组OS
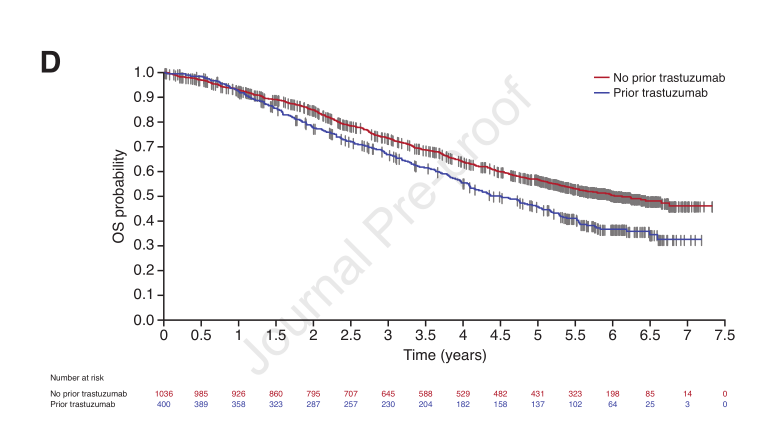
既往有无曲妥珠单抗OS
到最终数据截止时,679名患者(47%)报道了研究后的抗肿瘤治疗。最常用的抗HER2药物是曲妥珠单抗(25%)、曲妥珠单抗偶联物(19%)、拉帕替尼(16%)和帕妥珠单抗(7%)。最常用的化疗药物是卡培他滨 (20%)、长春瑞滨(10%)和紫杉类药物(6%)。最常见的内分泌治疗是芳香化酶抑制剂(8%)和抗雌激素(6%)。
综上,PERUSE研究的最终结果显示其安全性和有效性与CLEOPATRA研究类似,中位OS超过了5年。结果表明紫杉醇是一种有效的可替代多西他赛作为基础化疗药物。
原始出处:
Miles D, Ciruelos E, Schneeweiss A, et al; PERUSE investigators. Final results from the PERUSE study of first-line pertuzumab plus trastuzumab plus a taxane for HER2-positive locally recurrent or metastatic breast cancer, with a multivariable approach to guide prognostication. Ann Oncol. 2021 Jul 2:S0923-7534(21)02105-0. doi: 10.1016/j.annonc.2021.06.024. Epub ahead of print. PMID: 34224826.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#局部复发#
44
#PE#
45
#疗效和安全性#
37
#Oncol#
34
#曲妥珠#
37
#HER2阳性#
32
#转移性#
24
#局部#
33
谢谢梅斯提供这么好的信息,学到很多
0
谢谢梅斯分享这么多精彩信息
56