Sci Transl Med:军事医学研究院刘玮/曹务春团队在新发传染病领域获得重要进展
2018-09-22 佚名 病毒学界
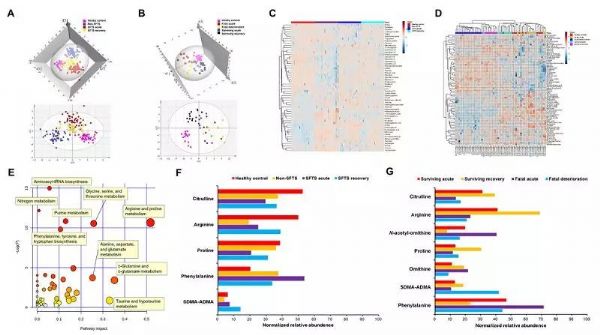
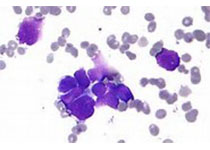
该研究首次报道了SFTS病毒感染中血小板数量下降及T淋巴细胞功能失调与精氨酸代谢异常有关。并经临床随机对照试验证实,补充精氨酸可以显着改善SFTS病例的相关临床指标。研究不仅从全新角度揭示了SFTS病毒的致病机理,而且为SFTS和其他病毒性出血热的临床治疗提供了崭新思路。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#TRA#
39
#重要进展#
33
#Transl#
34
#医学研究#
26
#Med#
23