NEJM:TSLP单抗Tezepelumab治疗严重不受控制哮喘III期临床研究获得成功
2021-05-13 MedSci原创 MedSci原创
对于严重、不受控制的哮喘患者,TSLP单抗Tezepelumab在降低恶化风险,改善肺功能、哮喘控制和健康相关生活质量方面显著优于安慰剂
临床上,大约10%的哮喘患者病情较为严重,在治疗后仍有症状,甚至加重。严重的、不受控制的哮喘发病率虽然较低,但医疗成本负担却十分沉重。Tezepelumab是一种人源的抗上皮细胞因子 (thymic stromal lymphopoietin,TSLP)单克隆抗体,通过阻止TSLP与受体复合物相互作用,从而阻止TSLP攻击的免疫细胞和释放促炎性细胞因子,进而防止哮喘恶化并控制哮喘。近日研究人员公布了Tezepelumab治疗严重,不受控制的哮喘患者III期临床研究结果。

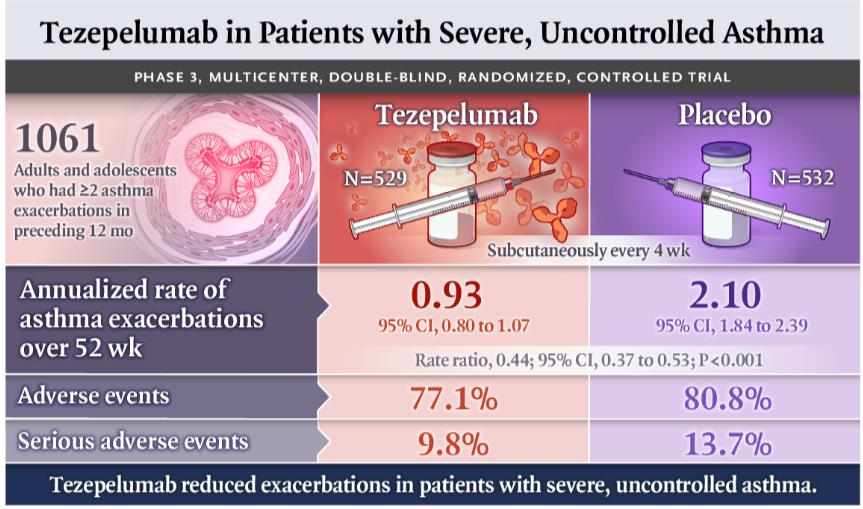
本次研究为III期、多中心、随机、双盲、安慰剂对照试验。12-80岁的严重,不受控制的哮喘患者参与,随机接受皮下注射Tezepelumab(210mg)或安慰剂,每4周一次,共52周。研究的主要终点是52周内哮喘恶化的年化率。次要终点包括1秒用力呼气量(FEV1)和哮喘控制问卷-6得分(ACQ-6;范围:0[无损害]至6[最大损害])、哮喘生活质量问卷得分(AQLQ;范围:1[最大损害]到7[无损害])以及哮喘症状每日得分(ASD;范围:0[无症状]到4[最严重的症状])。
1061名患者参与研究,其中529名接受Tezepelumab治疗,532名患者接受安慰剂治疗。Tezepelumab组哮喘加重的年化率为0.93,安慰剂组为2.10(比率为0.44)。在血液嗜酸性粒细胞计数低于每微升300的患者亚组中,Tezepelumab组恶化年化率为1.02,安慰剂为1.73(比率为0.59)。在第52周时,Tezepelumab对支气管扩张前FEV1的改善程度优于安慰剂(0.23 vs 0.09L),在ACQ-6评分 (-1.55 vs -1.22)、AQLQ评分(1.49 vs 1.15)以及ASD评分(-0.71 vs -0.59)改善方面优于安慰剂组。组间不良事件的发生率和类型无明显差异。
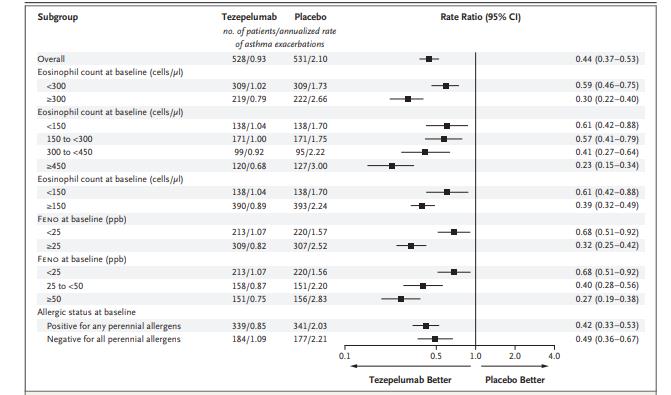
Tezepelumab vs 安慰剂对哮喘患者恶化风险的影响
研究认为,对于严重、不受控制的哮喘患者,TSLP单抗Tezepelumab在降低恶化风险,改善肺功能、哮喘控制和健康相关生活质量方面显著优于安慰剂。
原始出处:
Andrew Menzies-Gow et al. Tezepelumab in Adults and Adolescents with Severe, Uncontrolled Asthma. N Engl J Med, May 13, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#III#
31
#mAb#
28
#II期临床研究#
25
#III期临床研究#
43
#PE#
38
#I期临床#
25
#II期临床#
27
#III期#
31
#Tezepelumab#
29
#PEL#
35