JAMA Oncol:骨髓瘤维持治疗,哪个方案更优?
2018-08-19 肿瘤资讯编辑部 肿瘤资讯
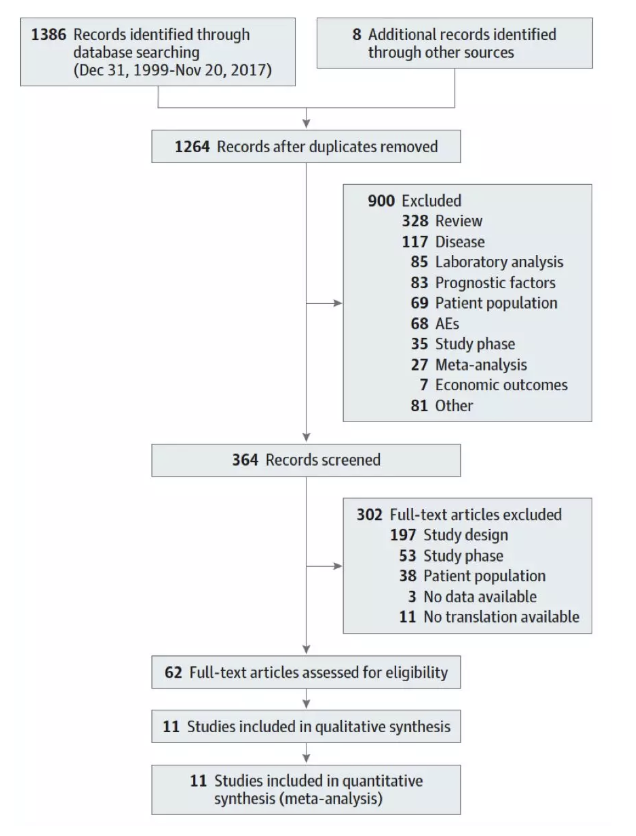
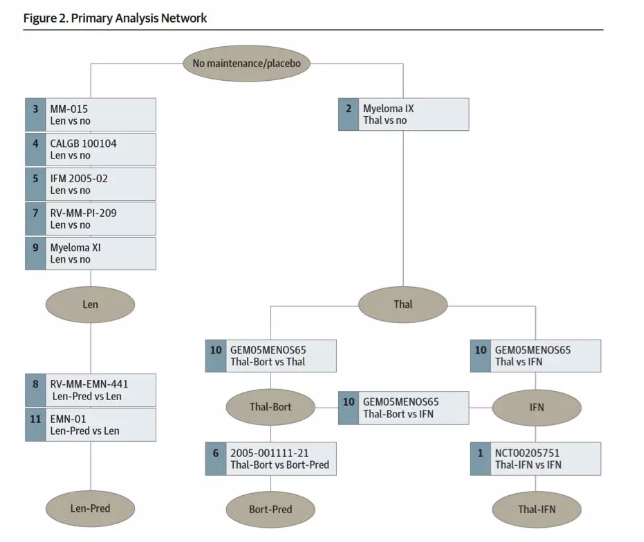
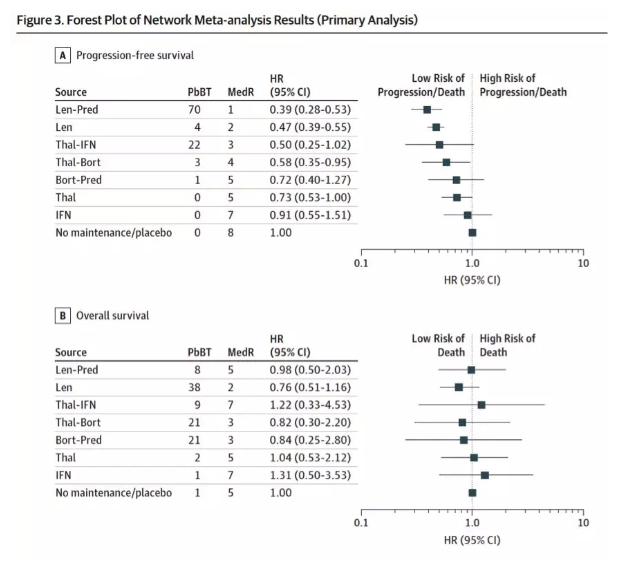
目前已有多项研究探索了多发性骨髓瘤(MM)的维持治疗。尽管研究结果提示维持治有一定疗效,但尚无证据显示何种维持治疗方案更优。近期,发布于JAMA Oncology杂志的一项荟萃分析,探讨了各个维持治疗方案对比无维持治疗或安慰剂维持的疗效,并在特定人群中进行了疗效对比。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Oncol#
35
好文章,谢谢分享!
90
好文章,谢谢分享!
89
好文章,谢谢分享!
70
好文章,谢谢分享!
73
好文章,谢谢分享!
0
好文章,谢谢分享!
40
好文章,谢谢分享!
36
好文章,谢谢分享!
39
好文章,谢谢分享!
28