尽管极早产儿,即胎龄少于28周的婴儿,相对较少,占全世界所有早产儿的5.2%。据数据显示,这些最不成熟的婴儿患各种并发症风险升高,包括支气管肺发育不良,脑出血,坏死性小肠结肠炎,败血症和视网膜病变等,且与长期不良结果相关。
极早产儿与全世界医疗保健系统的沉重负担有关。在发达国家,大型队列研究发现,在英国极早产儿的存活率为62%,法国为69%,挪威为74%,美国为72%。同时在过去的20年中,这些婴儿的生存结局得到了显著改善。然而,在中国,对于极早产儿的预后知之甚少。

pixabay
5月11日,发表在JAMA Network Open杂志的一项研究描述过去10年中国极早产儿的存活率和主要发病率。结果发现,在中国出生的极早产儿有着很高的死亡率和发病率。尽管随着时间的推移生存率有所提高,但主要发病率有所增加。
在这项研究中,来自复旦大学附属儿童医院新生儿科研究团队对来自2010年1月1日至2019年12月31日中国31个省的68个新生儿重症监护病房中的胎龄小于28周的婴儿进行分析,探索过去10年来中国极早产儿的存活率和主要发病率。
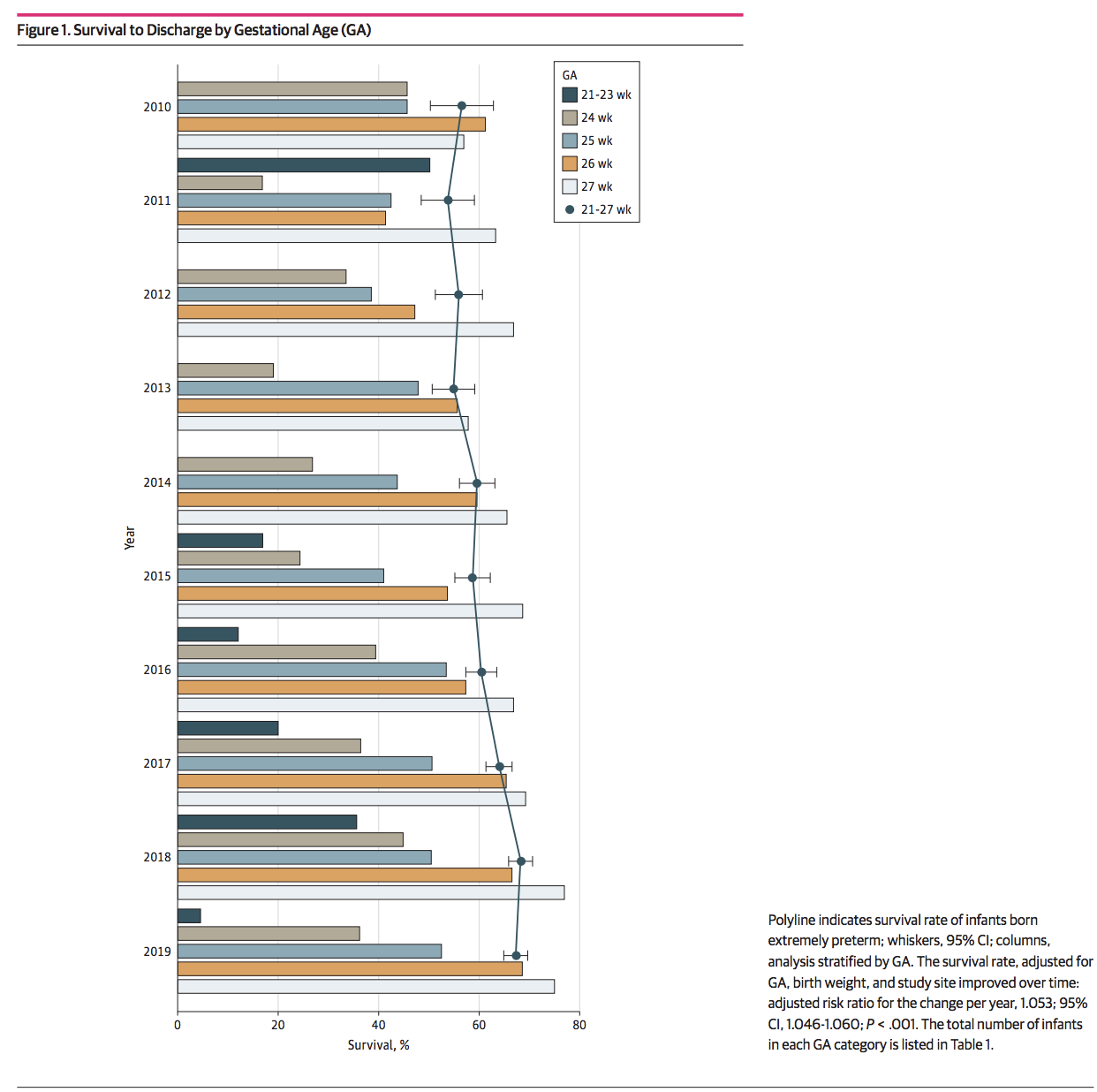
结果显示,在8514例符合条件的婴儿中,男性5295例(62.2%),5302例婴儿(62.3%)能够存活下来。其中,22周,23周,24周,25周,26周和27周的存活率分别为4.8%,18.3%,35.3%,48.6%,61.0%和69.1%。从2010年到2019年,对于27周极早产儿的存活率有了明显的提升,从56.4%提高到68.0%,对于24周以下出生的婴儿没有明显变化。
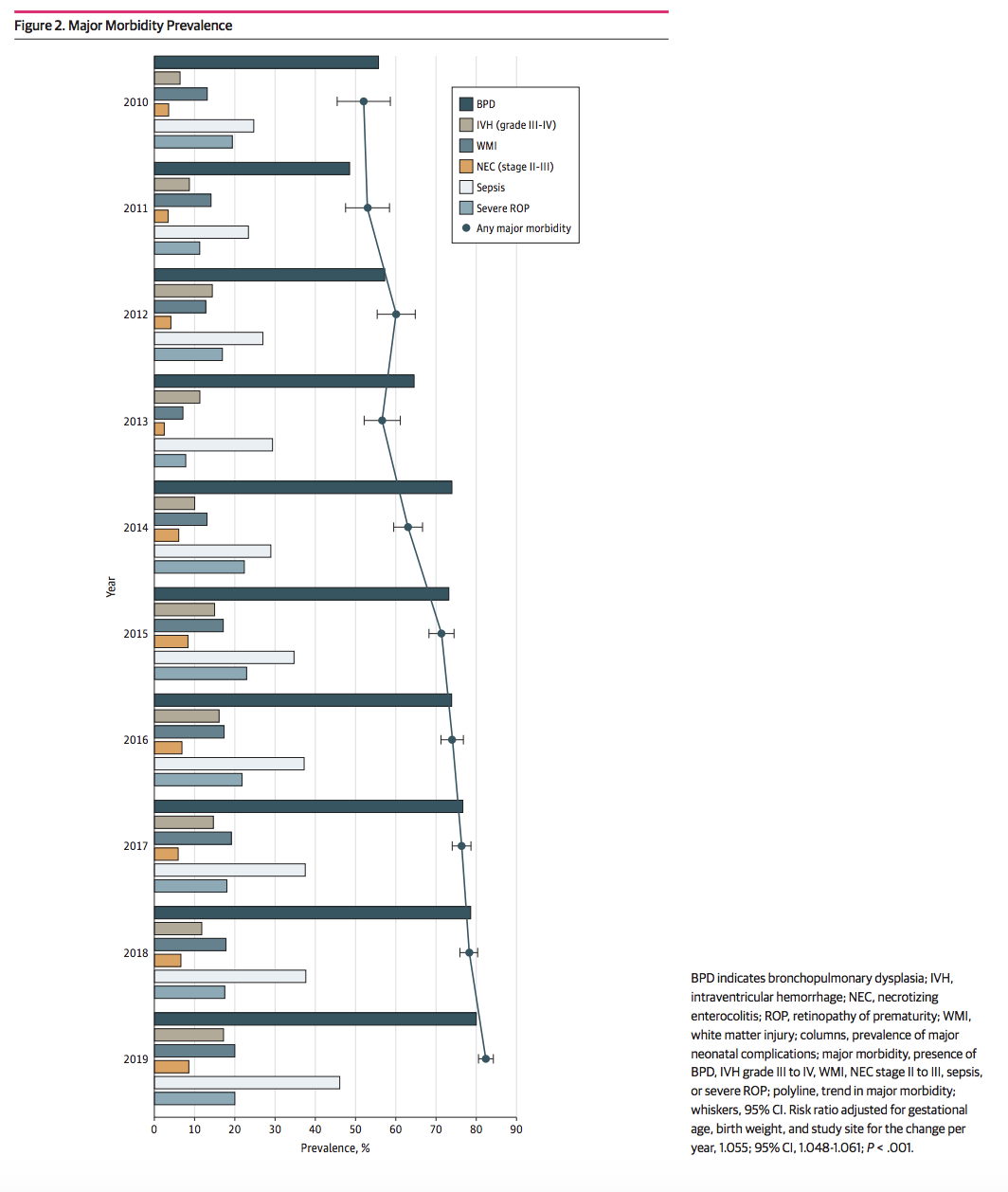
在重大疾病的发病率方面,在8281例婴儿中,有5999例发生了重大疾病,发病率为72.4%。从2010年到2019年,重大疾病的发病率从52.0%上升到82.3%。在5179例婴儿中,有3835例婴儿发生支气管发育不良(74.0%);在接受颅骨成像检查的7566例婴儿中,有1262例(16.7%)白质损伤,3691例婴儿(48.8%)患了脑出血。在8219例婴儿中,有830例婴儿发生坏死性小肠结肠炎(10.1%),其中,有531例婴儿被诊断出患有II至III期坏死性小肠结肠炎,57例发生了坏死性小肠结肠炎后狭窄。在8996例婴儿中,共有2996例(36.3%)患了败血症。在8281名婴儿中,共有4674名婴儿中进行了眼科检查(56.4%),在4674例婴儿中,共有有3060例婴儿(65.5%)达到了视网膜病变的诊断标准。在4518婴儿中,有848例婴儿患有严重的视网膜病变(18.8%)。
在对接受积极治疗的婴儿进行的多因素分析中,研究人员发现,出生体重,PROM和产前类固醇相关存活率有所提高。但是,多胎出生,男性,有妊娠糖尿病母亲和低Apgar得分与生存率降低有关。
总之,中国是一个人口稠密的国家,早产数量上排名全球第二。随着社会的进步,经济的发展和医疗水平的提高,极早产儿存活率提高,但合并症发病率增加。在中国,对极早产儿的照料已经成为亟需解决的问题。这项队列研究为中国大陆极早产儿的短期结局提供了有效而详细的信息。
原始出处
Zhicheng Zhu, MD1; Lin Yuan, MD1; Jin Wang, MD1; et al.Mortality and Morbidity of Infants Born Extremely Preterm at Tertiary Medical Centers in China From 2010 to 2019.JAMA Netw Open. 2021;4(5):e219382. doi:10.1001/jamanetworkopen.2021.9382
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#PE#
30
#发病率#
26
#NET#
40
#合并症#
41
#三级#
40
#极早产儿#
42
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
42