Eur Respir J :肺动脉高压的生理基础
2021-11-08 刘少飞 MedSci原创
肺动脉高压 (PAH) 是一种罕见的呼吸困难疲劳综合征,由肺血管阻力行性增加和最终右心室 (RV) 衰竭引起。PAH 中的 RV 通过增加收缩力来适应增加的后负荷,以保持其与肺循环的耦合。

PAH 的诊断依赖于排除导致肺动脉压 (PAP) 升高的心、肺或血栓栓塞性原因,随后右心导管插入术显示平均 PAP (mPAP) 高于 20 mmHg,楔形 PAP (PAWP) 低于或 等于 15 mmHg 且 PVR 等于或高于 3 Wood 单位。 在大约一半的情况下,PAH 是特发性 (IPAH)。 尽管过去几十年治疗取得了进展,但 PAH 仍然无法治愈。尽管存在广泛的肺血管重构,但 PAH 患者的肺功能通常得到良好保护,出现过度换气和生理死腔增加,但肺力学变化很小,仅轻度至中度低氧血症和低碳酸血症。
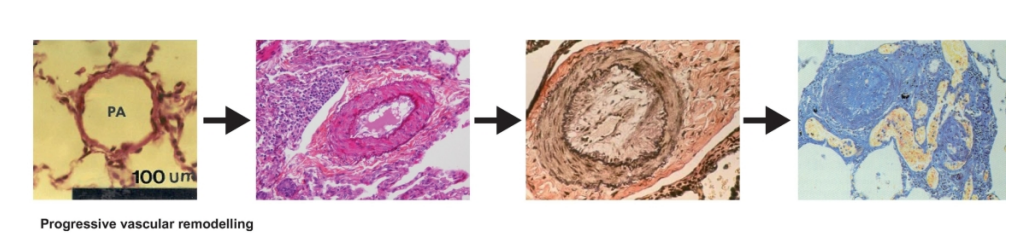
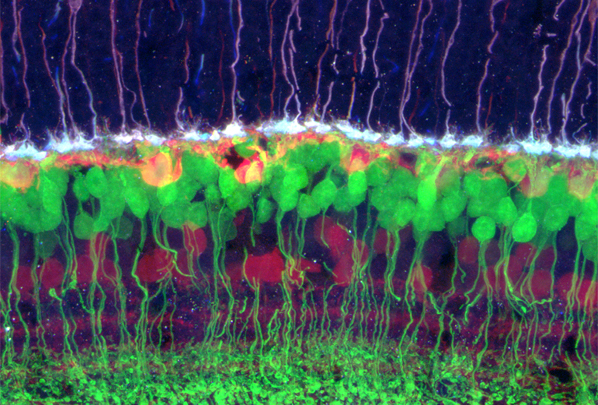
PAH 的组织病理学特征是小动脉内膜增生,演变为同心或偏心层状硬化、中层肥厚和外膜增生,伴有不同的炎症反应和偶见的纤维蛋白样坏死。晚期 PAH 可能与所谓的丛状病变有关,该病变包括通道增殖以及闭塞小动脉附近内皮细胞和炎症细胞的积累。丛状病变呈散在分布,多见于多支动脉,从大的肌肉甚至弹性肺动脉垂直产生的分支,与 PVR 增加无关,并且实际上在大约三分之二的患者中找不到。多达三分之一的 PAH 患者也可能发生微血栓病变,而且与 PVR 的增加没有明确的关系。中层肥大与急性前列环素诱导的 PVR 降低相关。
虽然肺循环在 PAH 中被广泛重塑,但这些患者的症状和结果在很大程度上取决于 RV 结构和功能的改变。本文将回顾 PAH 两个方面的生理基础,重点关注该病症的特发性形式,以避免合并症的混杂影响。
肺力学、通气和气体交换
PAH 中的肺功能测试显示,在严格确认的 IPAH 病例登记册中,没有或仅有轻微的肺一氧化碳弥散能力 (DLCO) 降低容量限制。 更现代的 PAH 登记处报告了 DLCO 更重要的下降,其中包括患有相关疾病、吸烟、临床无症状的心血管或呼吸系统疾病以及不太严格的血流动力学定义的老年患者。 晚期 PAH 患者的小气道阻力可能增加,这是动态过度充气和运动诱发的呼吸困难的原因。 也有呼吸肌力量降低的报道。 然而,肺力学和呼吸肌功能的这些改变似乎不会限制有氧运动能力。
PAH 中动脉血气分析的特征是氧和二氧化碳(PaO2 和 PaCO2)的动脉分压正常或降低。 如图下所示,大约一半患者的 PaO2 或 PaCO2 低于正常值,但严重低碳酸血症比严重低氧血症更常见。 低碳酸血症而非低氧血症是 IPAH 生存率降低的独立预测因素。 动脉血气、肺活量测定和 DLCO 在 IPAH 和慢性血栓栓塞性 PH (CTEPH) 中同样受到干扰,因此这些测量不能用于区分这两种情况。
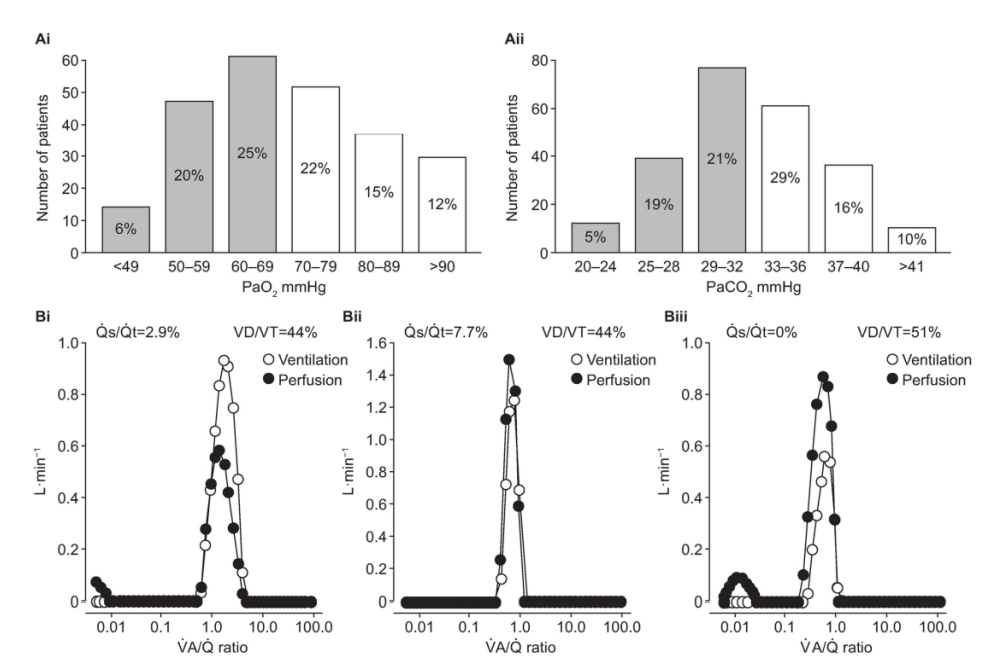
临床相关性。 PAH 中的肺气体交换出人意料地保存完好。 这些患者的过度换气和血气改变基本上是由心输出量减少、生理死腔增加和化学敏感性增加的组合来解释的。
肺循环:稳态血流动力学
肺血管阻力
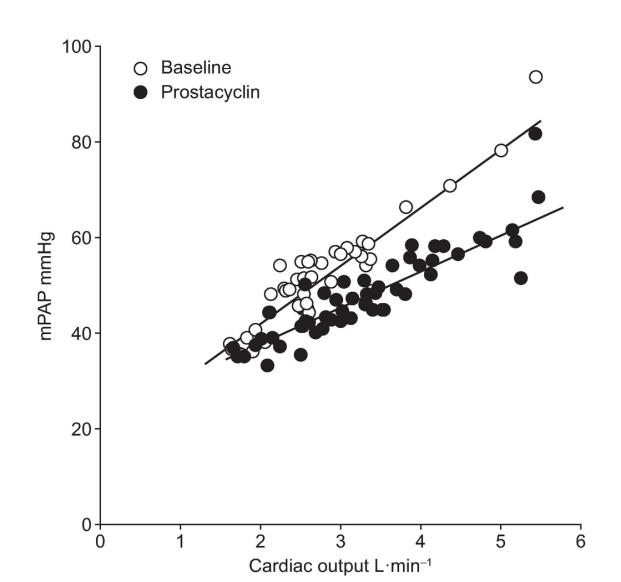
肺血管疾病的定义取决于 PVR。 然而,由于血流和压力引起的血管募集和/或扩张,PVR 会随着心输出量的增加而降低,因此,肺循环在 PAH 或左心衰竭时的肺循环阻力特性可以通过多点更好地定义 压力-流量关系。 这种方法已被用于阐明前列环素治疗对 PAH 的影响。 在该研究中,肠外依前列醇降低了 mPAP-心输出量关系的斜率,而静息 PVR 保持不变(图下)。
PVR的分区
测量 PAWP 的 PA 球囊闭塞后的压力衰减曲线呈现出快速部分,对应于上游动脉阻力,而缓慢部分对应于包含小动脉、毛细血管和静脉的下游阻力。纯近端 CTEPH 中的上游 PVR 增加。 PAH 和肺静脉闭塞性疾病 (PVOD) 的下游 PVR 增加。
右心室功能:心室-动脉耦合
尽管存在明显的胚胎学和结构差异,但 RV 和 LV 的机械特性相似。 所谓的“内心法则”同样适用于两者。 心室对增加的后负荷的即时适应是通过遵循 Starling 心脏定律增加的尺寸。 然而,这种“异量”反应在几分钟内被“等量”增加的收缩力所取代,遵循 Anresp 的心脏定律,允许保留的流量输出而不会扩张和增加填充压力。心室肥大加强了长期的等势适应。 当等距适应耗尽时,异量适应再次开启以保持心输出量,但代价是心室扩张和上游阻塞。RV 功能与后负荷的耦合具有不可避免的舒张成分。如图下所示,舒张功能由舒张弹性曲线描述,该曲线可以由一系列压力-容积环在可变负荷下确定,也可以通过在单个 PV 环上拟合收缩末期和舒张末期 PV 关系来确定。
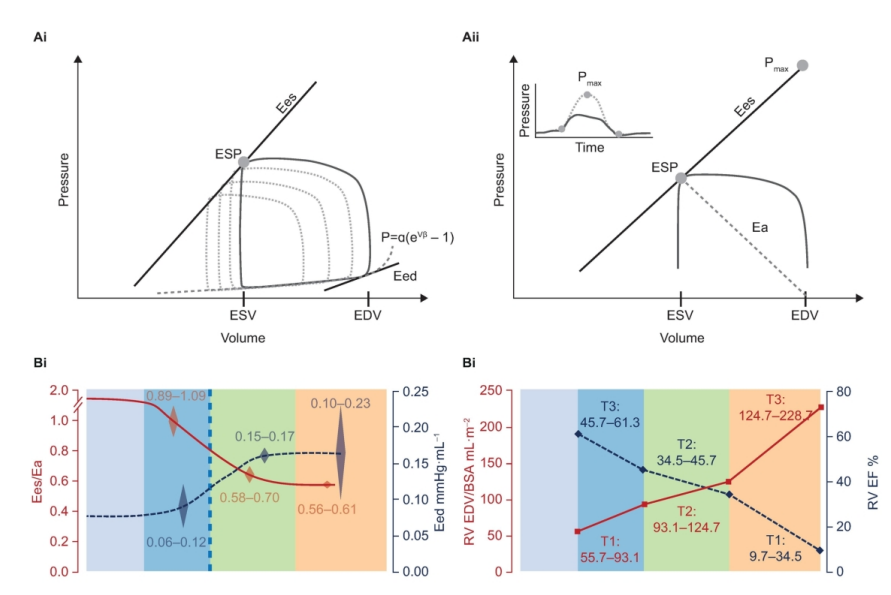
由于 RV 功能是 PAH 症状和结果的主要决定因素,因此正在开发简单的非侵入性评估方法。 其中之一是 TAPSE(估计 Ees)与 sPAP(估计后负荷)的比率,这在标准多普勒超声心动图期间很容易测量。 TAPSE/sPAP 比值已针对 Ees/Ea 比值的有创测量进行了验证,并显示出与心力衰竭和 PAH 的预后相关。
然而,PAH 的生理基础超出了 RV 功能障碍。 PAH 患者的管理需要彻底了解肺力学的基本生理学、肺气体交换、肺血管功能以及右心与肺循环的耦合。 这些知识不仅对于正确评估治疗干预至关重要,而且对于评估对该疾病的细胞和分子生物学快速增长的理解的临床相关性也是必不可少的。
参考文献:
Naeije R, Richter MJ, Rubin LJ. The physiologic basis of pulmonary arterial hypertension. Eur Respir J. 2021 Nov 4:2102334. doi: 10.1183/13993003.02334-2021. Epub ahead of print. PMID: 34737219.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#生理基础#
43
#动脉高压#
37
学习了,很好
52
好文章,谢谢分享。
62
优秀,学习了
57
不错
49