Cardiovasc Diabetol:累积甘油三酯-葡萄糖指数越高,心血管疾病风险越大!
2022-02-20 Nebula MedSci原创
发生心血管疾病的风险随着累积TyG指数的增加而升高
既往研究表明,基线甘油三酯-葡萄糖 (TyG) 指数与心血管疾病 (CVD) 之间存在显著关系。但是,TyG 指数和新发心血管疾病的长期相关性仍不确定。本研究旨在探讨累积 TyG 指数与心血管疾病风险之间的关系。
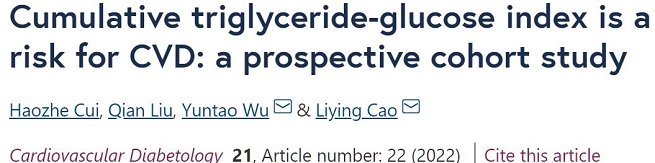
在这项研究中,招募了 2006 年至 2013 年参加 Kailuan 研究、连续四次检查中没有卒中、心肌梗塞和癌症的个体。通过将平均 TyG 指数乘以两次连续检查之间的时间来计算累积 TyG 指数。根据累积 TyG 指数水平将所有受试者分为四个四分位数组:Q1 组,≤ 50.65(作为参考组);Q2 组,50.65-53.86,Q3 组,53.86-57.44;Q4 组,>?57.44。采用多变量 Cox 比例风险模型估计累积 TyG 指数与心血管疾病风险之间的相关性。
不同累积TyG指数水平个体发生心血管疾病的风险
本次分析共纳入了 44,064 位受试者。中位随访了 6.52±1.14 年后,分别有 2057 位、395 位和 1695 位个体发生过心血管疾病、心肌梗塞和卒中。根据多重潜在的混杂因素调整后,发生心血管疾病的风险随着累积TyG指数的增加而升高,与 Q1 组相比,Q2 组、Q3 组和 Q4 组的风险比(HR)分别是 1.25 (1.08-1.44)、1.22 (1.05-1.40) 和 1.39 (1.21–1.61)。
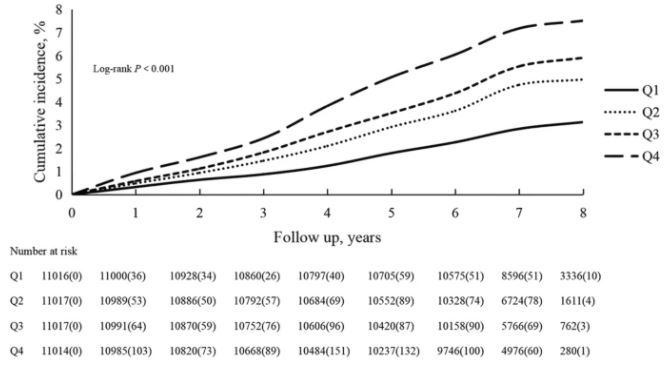
不同较高累积TyG指数水平暴露时间个体发生心血管疾病的风险
此外,较高 TyG 指数暴露的持续时间较长也与心血管疾病风险增加显著相关。在亚组和敏感性分析中也获得了类似的结果。
综上所述,累积 TyG 指数与心血管疾病风险增加密切相关。将甘油三酯和空腹血糖维持在理想范围内,更好地控制累积 TyG 指数对于预防心血管疾病很重要。
原始出处:
Cui, H., Liu, Q., Wu, Y. et al. Cumulative triglyceride-glucose index is a risk for CVD: a prospective cohort study. Cardiovasc Diabetol 21, 22 (2022). https://doi.org/10.1186/s12933-022-01456-1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#DIA#
44
#BET#
56
#ASC#
0
#疾病风险#
52
#血管疾病#
35
学习
80