脊髓外硬脊膜内肿瘤切除术
2016-03-14 MedSci www.windrug.com
脊髓外硬脊膜内肿瘤切除术 脊髓外硬脊膜内肿瘤约占脊髓瘤的55%~67%,主要系神经根的神经鞘瘤(神经纤维瘤)和脊膜瘤。这两种都是有包膜的良性肿瘤,切除后可以根治,手术中必须想尽一切办法完全切除。 神经鞘瘤切除术 神经鞘瘤与脊髓的关系可有3种情况:①位于脊髓背侧;②位于脊髓腹侧或侧前方;③哑铃形肿瘤。 椎板减压、脊髓探查以及硬脊膜外肿瘤切除的原则均适用于本肿瘤。为避免重复,仅将不同的手
脊髓外硬脊膜内肿瘤切除术
脊髓外硬脊膜内肿瘤约占脊髓瘤的55%~67%,主要系神经根的神经鞘瘤(神经纤维瘤)和脊膜瘤。这两种都是有包膜的良性肿瘤,切除后可以根治,手术中必须想尽一切办法完全切除。
神经鞘瘤切除术
神经鞘瘤与脊髓的关系可有3种情况:①位于脊髓背侧;②位于脊髓腹侧或侧前方;③哑铃形肿瘤。
椎板减压、脊髓探查以及硬脊膜外肿瘤切除的原则均适用于本肿瘤。为避免重复,仅将不同的手术注意点介绍如下:
(一)脊髓背侧的神经鞘瘤
 |
 |
| 1-1 切开硬脊膜显露肿瘤 | 1-2 肿瘤切除后示脊髓受压征 |
| 图1 脊髓背侧神经鞘瘤切除术 | |
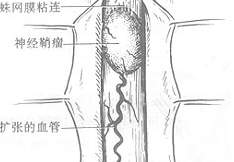
完成肿瘤部位的椎板切除后,在硬脊膜外即可看到及扪到硬脊膜局限性膨出,切开硬脊膜即可见肿瘤。肿瘤呈圆形或椭圆形,与一神经后根相连。伴随该神经根的动脉即系供应肿瘤的血管。肿瘤可为实质性,也可为囊性变[图1-1];如为囊性变,用细针穿刺抽液即可瘪缩而利于剥离。切除时先切开肿瘤周围的蛛网膜再剥离瘤体,于肿瘤一端缝一牵引线并向上牵引,用剥离子轻轻分离到瘤蒂,在血管处上银夹或丝线结扎或双极电凝烧灼后剪断,即可把肿瘤取出,颈膨大或腰膨大处神经根要尽量保留。瘤床上可见局部血管明显变细或有血栓形成、脊髓变形及水肿[图1-2]。由此可见脊髓压迫症的预后与手术的早晚及脊髓压迫是否能完全解除有密切关系。术中应注意冲洗及吸引器不能直接作用于脊髓上,必须先垫以带线脑棉片,用吸引器轻吸脑棉片。止血可用双极电凝。
(二)脊髓前方及侧前方的神经鞘瘤
 |
| 2-1 肿瘤在脊髓前方 |
切开硬脊膜后不能看到或不完全看到肿瘤[图2-1],但小心把脊髓的一侧推开即可窥见肿瘤的边缘。在推开脊髓前必须用脑棉片妥为保护,牵拉要轻柔。然后剪断肿瘤侧的上、下齿状韧带,轻轻翻脊髓。剪开蛛网膜后,用细软剥离子分离,并用缝线轻轻牵引肿瘤。如系带蒂型者则易于提出,然后按脊髓背侧神经鞘瘤切除方法切了作之[图2-2]。如肿瘤基部很广或与前方粘连明显,则可剪断齿状韧带,轻翻脊髓,尽量把肿瘤显露后纵形切开包膜,用刮匙或活组织钳伸入囊内分块切除肿瘤[图2-3]。止血后尽量切除包膜,残留部分以双极电凝烧灼。必须注意位于脊髓正前方的某些神经鞘瘤易被误诊为脊髓内肿瘤,应切断齿状韧带并翻转脊髓仔细探查后才能给予正确诊断及治疗。
 |
 |
| 2-2 包膜外切除 | 2-3 脊髓前方及侧前方的神经鞘瘤切除术 |
| 图2 脊髓前方及侧前方的神经鞘瘤切除术 | |
哑铃形脊髓瘤绝大多数系神经鞘瘤,极少数为软骨瘤或骨瘤,其手术方法均相同。神经鞘瘤多发生于椎管内的神经后根处,可沿椎间孔蔓延至椎管外呈哑铃形。在胸部可进入后纵隔,在颈部可表现为颈部肿物[图3]。
 |
| 图3 哑铃形神经鞘瘤(横断面) |
作椎旁切口。切开皮肤后,在椎管内及椎旁分为两个显露途径,分别取出哑铃形肿瘤的两部分。如纵隔或颈部的肿瘤很大,病人不能于一次手术负担两处切除时,可分两期手术。
 |
 |
| 4-1 椎旁切口 | 4-2 切开硬脊膜,显露椎管内肿瘤 |
1.切口 以病灶为中心,距棘突约3cm左右,作纵形或弧形切口[图4-1]。
 |
 |
| 4-3 椎管内肿瘤切除后 | 4-4 缝合硬脊膜 |
2.肿瘤椎管内部分的切除 切开皮肤后,潜形向棘突处(即背正中线)分离。按椎板切除术的步骤切除椎板,将硬脊膜显露、剪开,分离肿瘤[图4-2],把肿瘤的椎管内部分切除[图4-3],并试把突向椎间孔外的肿瘤拉入椎管内切除。如肿瘤突出较大,不能拉入时,可用钝器把椎间孔的肿瘤残端向外推出。硬脊膜缺损如较小,可以直接缝合[图4-4],如缺损较大,则用筋膜修复[图4-5]。
 |
 |
| 4-5 用筋膜修复脊膜缺损 | 4-6 切开斜方肌 |
3.肿瘤椎管外部分的切除(哑铃形神经鞘绝大多数发生在胸椎,故以此为例说明)在原皮肤切口下切开斜方肌及菱形肌,拉开骶棘肌,结扎小血管,显露肋骨及横突[图4-6~8]。根据肿瘤大小决定切除肋骨的数目(一般不超过2~3根)。骨膜下剥离,切除选定的肋骨脊柱端约4~6cm及脊椎横突,结扎及切断肋间血管、神经及肌束,推开胸膜,显露肿瘤,分离四周的粘连即可将肿瘤剔出[图4-9]。
 |
| 4-7 拉开骶棘肌 |
 |
| 4-8 显露、切除肋骨 |
 |
| 4-9 分离并显露肿瘤 |
| 图4 胸段脊髓哑铃形神经鞘瘤切除术 |
脊膜瘤切除术
脊膜瘤自硬脊膜长出,大多在脊髓背侧或外侧,少数可在脊髓腹侧,基底一般都较广。如在脊髓背侧者,先把肿瘤与脊髓分开,然后连同肿瘤附着的硬脊膜一并切除,用双极电凝止血[能看图1-1、2]。缺损的硬脊膜可用筋膜修复[图4-5]。如缺损不大,也可不修复,但肌层要紧密缝合。小部分硬膜瘤痊于脊髓前方而基底又宽大者,只能剪开相应的齿状韧带[图2-2],轻轻翻转和保护脊髓后,用双极电凝烧灼开脊膜瘤的包膜,用刮匙或活组织钳咬除肿瘤内容物[图2-3]。然后尽量剪去已显露的包膜及其附着的硬脊膜。腹侧脊膜的缺损可不必修复。
[术中注意事项]
1.神经鞘瘤周围常有蛛网膜囊肿,手术中切勿仅满足于处理蛛网膜囊肿而遗漏瘤体,应仔细探查,确认无肿瘤时方可中止手术。
2.对范围较广泛哐与脊髓分界不清的肿瘤如结核瘤、脂肪瘤等,不可勉强分离,最好术中作冰冻切片,确定病理性质,根据其性质行全切除、大部切除或椎板切除减压等。
3.肿瘤椎管外部分切除时,切除肋骨后推开胸膜时,注意防止胸膜损伤造成气胸。如果采用硬脊膜外麻醉而气胸较重时,病人可能呼吸困难。因此,此类手术以选用气管插管全麻较好,术终请麻醉师扩肺,排除胸腔积气;如残留气体较多,术后可于第二肋间锁骨中点处行闭式引流。
[术后处理]
同椎管-脊髓探查术。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#切除术#
36
#肿瘤切除#
38
学以致用
113
内容精彩
127
#硬脊膜#
39