Circulation:IL-10-STAT3-半乳凝素-3轴对心肌梗死后产生OPN的修复性巨噬细胞极化至关重要
2018-11-03 MedSci MedSci原创
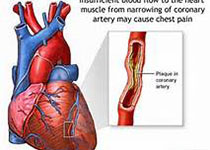
现已知骨桥蛋白(OPN)和半乳凝素-3均参与伤口愈合过程中死亡细胞的吞噬清除和修复性纤维化;CD206+巨噬细胞通过吞噬和纤维化参与心肌梗死(MI)后的组织修复。但OPN、半乳凝素-3和巨噬细胞极化在MI环境中的关系尚不明确。心肌梗死后第3天,心肌Spp1(编码OPN的基因)出现明显的激活。为明确心肌梗死后,Spp1的转录活性在哪种细胞中增强,研究人员对心肌梗死后第3天的EGFP-Spp1敲进(K
心肌梗死后第3天,心肌Spp1(编码OPN的基因)出现明显的激活。为明确心肌梗死后,Spp1的转录活性在哪种细胞中增强,研究人员对心肌梗死后第3天的EGFP-Spp1敲进(KI)受体小鼠进行分析。结果显示Spp1的转录活性仅在梗死心肌内的CD206+巨噬细胞中增强,而且大部分CD206+巨噬细胞在心肌梗死后有较强的Spp1转录激活。
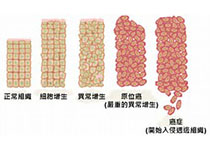
梗死心肌的巨噬细胞中Lgal3(编码半乳凝素-3)的时间表达谱与Spp1相似,OPN几乎完全由半乳凝素-3[hi]CD206+巨噬细胞产生。既往报道IL-4和IL-10可促进CD206+巨噬细胞介导的心梗后的心肌修复,但本研究显示仅IL-10可刺激CD11b+Ly6G-细胞分化成产生OPN的半乳凝素-3[hi]CD206+巨噬细胞,表现出增强的吞噬能力,而IL-4无此效应。抑制STAT3酪氨酸磷酸化可抑制IL-10诱导的胞内半乳凝素-3的表达和Spp1的转录激活。敲低半乳凝素-3可抑制其分化成产生OPN的细胞,但STAT3激活不能。STAT3的酪氨酸磷酸化和半乳凝素-3[hi]CD206+细胞在Spp1敲除小鼠的心脏CD11b+Ly6G-细胞上的出现率均与在野生型小鼠中的一致。Spp1敲除小鼠易出现心梗后左心室扩张,而且梗死心肌中TUNEL标记的阳性细胞(即凋亡细胞)也多于野生型小鼠的。
OPN几乎完全是由半乳凝素-3[hi]CD206+巨噬细胞产生,特别是在心肌梗死后的梗死心肌中。IL-10-STAT3-半乳凝素-3轴是心肌梗死后产生OPN的修复性巨噬细胞极化的关键,这些巨噬细胞通过促进纤维化和凋亡细胞清除促进组织修复。本研究表明半乳凝素-3或可通过控制OPN水平促进梗死心肌的修复性纤维化。
Kohsuke Shirakawa,et al. IL (Interleukin)-10–STAT3–Galectin-3 Axis Is Essential for Osteopontin-Producing Reparative Macrophage Polarization After Myocardial Infarction. 24 Jul 2018. Circulation. 2018;138:2021–2035
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#OPN#
40
#STAT3#
35
#IL-1#
39
#IL-10#
42
#细胞极化#
41
了解一下,谢谢分享!
55
谢谢分享学习
39