Br J Cancer:CDK4/6抑制剂在恶性胸膜间皮瘤临床前模型中的疗效分析
2021-10-27 xiaozeng MedSci原创
恶性胸膜间皮瘤(MPM)是一种进袭性、局部侵袭性且无法治愈的胸膜恶性肿瘤,其发病与工作上接触石棉相关。
恶性胸膜间皮瘤(MPM)是一种进袭性、局部侵袭性且无法治愈的胸膜恶性肿瘤,其发病与工作上接触石棉相关。尽管许多国家已禁止使用石棉,但石棉绝缘建筑仍遍布世界各地,一些国家仍在制造和使用大量石棉。
既往研究显示,在约10-15%的MPM患者中发现了BAP1和其他癌症易感基因(如PALB2、BRCA2、CHEK2和MLH1等)的遗传突变。
目前对于晚期MPM患者的治疗选择有限。顺铂联合培美曲塞(pemetrexed)已成为晚期MPM患者的标准治疗策略。在化疗中加入贝伐单抗(bevacizumab)可适度改善总生存期,但并非所有国家都采用这种治疗策略。
在最近的一项针对晚期NSCLC的个性化治疗的临床试验中,研究人员发现,CDKN2A缺失与患者对CDK4/6抑制剂的敏感性相关。而高频率的CDKN2A缺失以及细胞周期失调是MPM的标志时间,因此CDK4/6抑制剂或可成为MPM的一种新治疗方法。
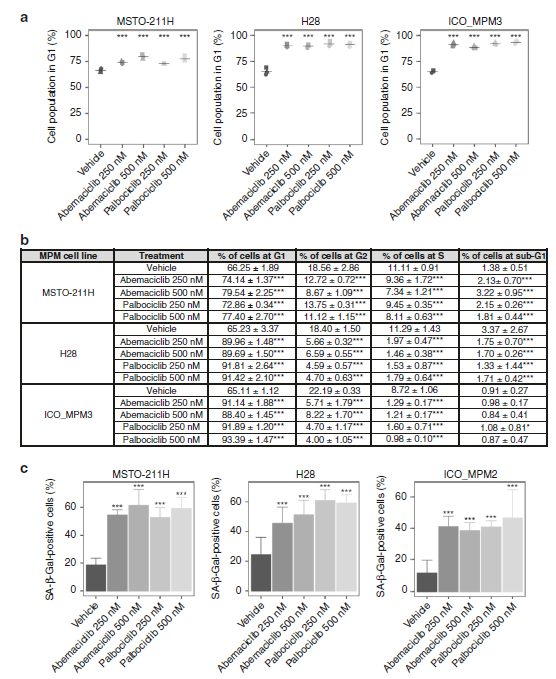
CDK4/6抑制剂对MPM细胞周期和衰老的影响
该研究旨在揭示CDK4/6抑制剂在MPM临床前模型中的抗肿瘤功效,并研究其在MPM治疗中的潜力。研究人员还通过分析公开可用的MPM转录组数据评估了CDK4或CDK6过表达在MPM患者原发性肿瘤中的预后影响。
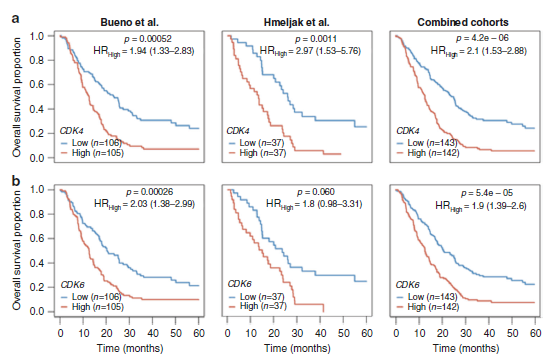
结果显示,CDK4或CDK6过表达状态的患者的总生存期较短。在所有评估的细胞模型中,采用100 nM的阿贝西利(abemaciclib)或帕博西尼(palbociclib)处理能够显著降低细胞增殖作用。上述两种CDK4/6抑制剂均能够显著诱导细胞周期阻滞于G1期,进而促进细胞衰老并增强了MPM培养模型中的干扰素信号和肿瘤抗原呈递过程。在体临床前研究显示,在MPM移植瘤的无胸腺小鼠模型中给予帕博西尼可显著降低肿瘤的生长并延长小鼠的总生存期。
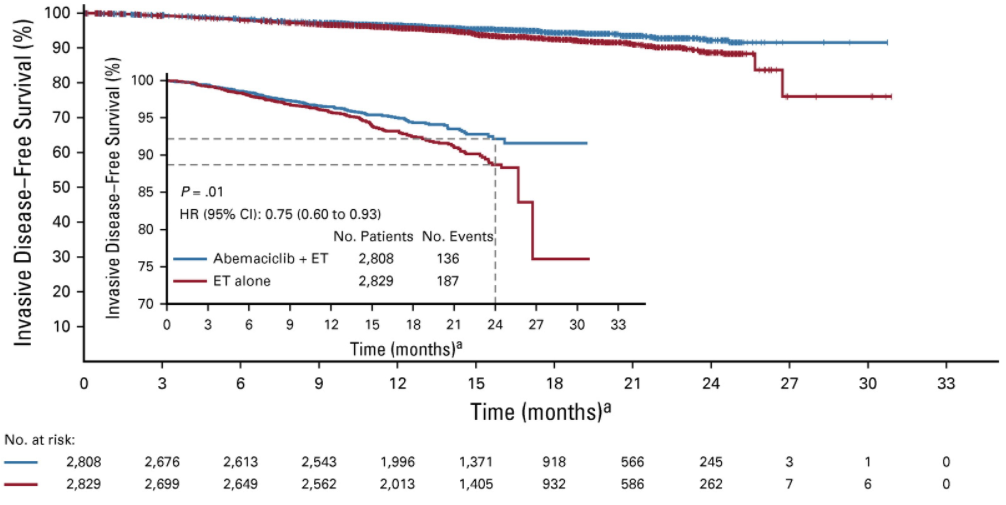
不同CDK4和CDK6表达水平的两组MPM患者的总体生存率
总而言之,该研究结果揭示,CDK4/6抑制剂主要是通过促进细胞周期在G1期的停滞并促进细胞衰老来降低MPM细胞的增殖。该临床前研究也为临床上评估CDK4/6抑制剂对MPM的疗效提供了一定的理论证据。
原始出处:
Aliagas, E., Alay, A., Martínez-Iniesta, M. et al. Efficacy of CDK4/6 inhibitors in preclinical models of malignant pleural mesothelioma. Br J Cancer (29 September 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#疗效分析#
39
#抑制剂#
41
#胸膜#
47
#CDK4#
32
#CDK#
40
#CDK4/6#
38
#间皮瘤#
33
MPM
70
西方国家中包括贲门腺癌在内的食管腺
45
学习学习
55