JACC:周转再加快——急性心梗低风险患者,PCI术后早期出院不影响结局!
2021-12-14 MedSci原创 MedSci原创
通过使用由结构化的多学科虚拟随访计划支持的路径,选定的低风险患者可以在成功的初级PCI之后安全出院。
在美国,每年约有500000名患者接受经皮冠状动脉介入治疗(PCI),整体花费可达到50亿美元。由于PCI操作后可能出现血管通路并发症或血管闭塞导致的急性冠状动脉缺血事件,PCI患者通常需要在医院过夜观察。
但是这种不良事件的发生风险正随着抗栓治疗的发展与冠状动脉支架的使用而逐渐降低,因此可以考虑于择期PCI术后当日出院,从而增加床位使用率、降低成本及院内感染的发生率。
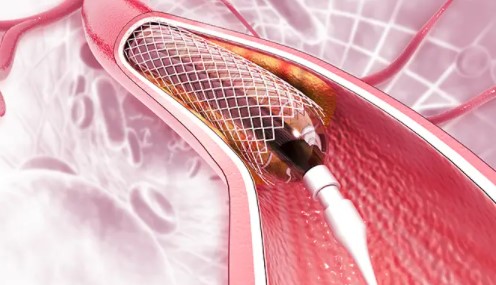
全球范围内,区域性心脏病发作服务通过初级经皮冠状动脉介入促进早期再灌注,改善了ST段抬高型心肌梗死(STEMI)的临床结果。一次性经皮冠状动脉介入治疗后的早期出院受到了患者的欢迎,并提高了医疗服务的效率。
为了评估针对低风险STEMI患者的新型早期出院路径的安全性和可行性,来自英国伦敦玛丽皇后大学威利安-哈维研究所心血管医学中心的专家开展了相关研究,结果发表在《美国心脏病学会杂志》JACC上。
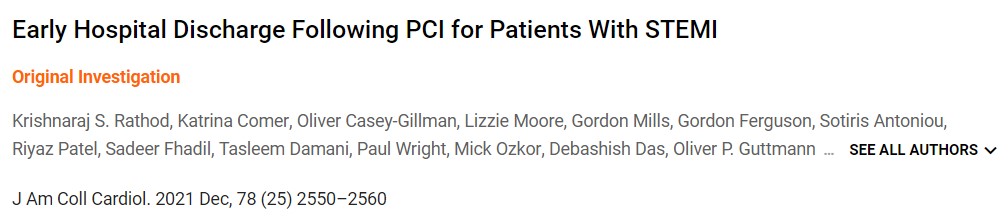
在2020年3月至2021年6月期间,600名被认为是早期主要不良心血管事件(MACE)低风险的患者被选入该路径,并在<48小时内成功出院。患者在出院后48小时由心脏康复护士进行结构化的电话随访,并在2、6、8周和3个月后进行虚拟随访。
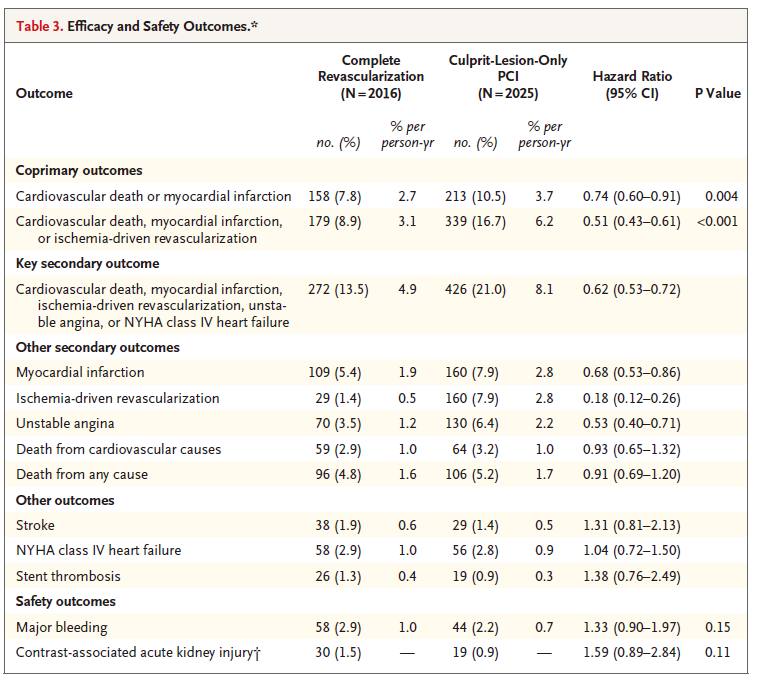
住院时间的中位数是24.6小时(四分位数范围[IQR]:22.7-30.0小时)(路径前中位数:65.9小时[IQR:48.1-120.2小时])。出院后,所有患者都被联系上,没有人失去随访。在271天(IQR:88-318天)的中位随访期间,有2例死亡(0.33%),都是由2019年(出院后>30天)的冠状病毒疾病引起的,心血管死亡率为0%,MACE率为1.2%。
总的来说,这一发现与既往符合路径标准的700名住院时间>48小时的患者(>48小时对照组)相比,在未经调整的分析和倾向匹配的分析中都是有利的(死亡率,0.7%;MACE,1.9%)。
早期出院与48小时候出院患者MACE及死亡率比较
综上,通过使用由结构化的多学科虚拟随访计划支持的路径,选定的低风险患者可以在成功的初级PCI之后安全出院。
参考文献:
Early Hospital Discharge Following PCI for Patients With STEMI. J Am Coll Cardiol. 2021 Dec, 78 (25) 2550–2560
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












很有帮助
42
#PCI术#
0
#JACC#
32
#急性心梗#
52
#ACC#
35
#PCI术后#
46
学习
54