Nat Med:为应对奥密克戎变异株加强针该选CoronaVac还是BNT162b2疫苗?
2022-01-21 MedSci原创 MedSci原创
主要接种CoronaVac疫苗的国家应考虑使用mRNA疫苗来加强免疫以应对奥密克戎变异株的传播。迫切需要进一步的研究来评估不同疫苗对奥密克戎变异株的有效性。
2021年11月,南非首次报道了一种具有更高传播能力的新型SARS-CoV-2变异株,命名为奥密克戎变异株(B.1.1.529的BA.1亚系)。奥密克戎变异株正迅速成为全球流行的主要SARS-CoV-2病毒,该变异株在病毒的刺突蛋白中有37个氨基酸被取代,其中15个位于受体结合域中。病毒中和抗体是保护人类面受病毒感染的主要决定因素。已有研究报道了与防止再感染或严重疾病相关的中和抗体阈值。尽管CD8T细胞已被证明具有保护作用,但让不能量化保护的相关性。

近日,顶级医学期刊Nature Medicine上发表了一篇研究文章,研究人员之前已经明确在活病毒检测中,50%的蚀斑减少中和(PRNT50)抗体滴度≥25.6,其对应于50%保护免受野生型(WT)SARS-CoV-2感染的阈值。
与野生型病毒相比,在接种两剂BNT162b2(GMT218.8)或CoronaVac疫苗(GMT32.5)后3-5周,研究人员发现针对奥密克戎变异株的血清抗体滴度显著降低(几何平均滴度(GMT)<10)。
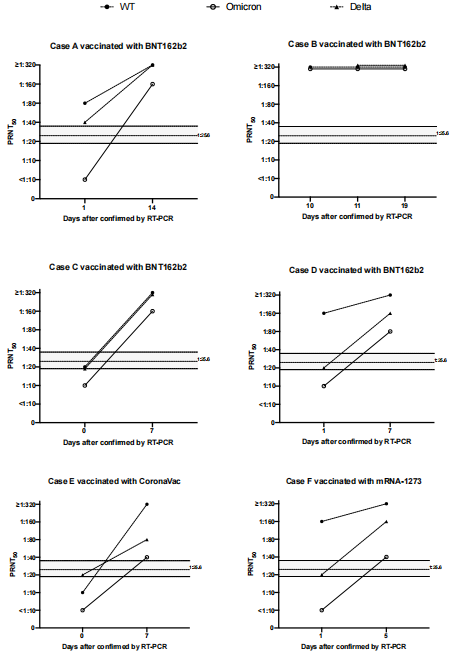
在之前接种过2剂BNT162b2疫苗的个体(25人中的22人)和之前接种过CoronaVac疫苗的个体(30人中的24人)中,88%的受试者(25人中的22人)在BNT162b2加强剂量后针对奥密克戎变异株PRNT50滴度≥25.6。然而,很少(3%)既往感染过的个体(30人中有1人)或接种了三剂CoronaVac疫苗的人(30人中有1人)达到了这个阈值。
该研究的结果表明主要接种CoronaVac疫苗的国家应考虑使用mRNA疫苗来加强免疫以应对奥密克戎变异株的传播。迫切需要进一步的研究来评估不同疫苗对奥密克戎变异株的有效性。
原始出处:
Samuel M. S. Cheng,et al.Neutralizing antibodies against the SARS-CoV-2 Omicron variant following homologous and heterologous CoronaVac or BNT162b2 vaccination.Nature Medicine.2022.https://www.nature.com/articles/s41591-022-01704-7
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Nat#
35
#变异#
30
#Med#
23