NEJM:达洛鲁胺对转移性激素敏感性前列腺癌生存率的影响
2022-03-24 MedSci原创 MedSci原创
达洛鲁胺、雄激素剥夺疗法和多西他赛联合治疗的总生存期明显长于安慰剂加雄激素剥夺疗法和多西他赛,并且加用达洛鲁胺导致关键次要终点有所改善。两组的不良事件发生率相似。
达洛鲁胺是一种有效的雄激素受体抑制剂,与非转移性去势抵抗性前列腺癌患者的总生存期增加相关。达洛鲁胺、雄激素剥夺疗法和多西他赛的组合是否会增加转移性、激素敏感性前列腺癌患者的生存率尚未明确。
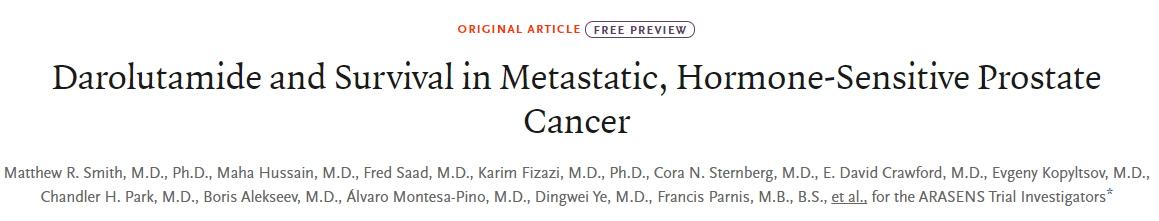
近日,顶级医学期刊NEJM上发表了一篇研究文章,在这项国际3期试验中,研究人员将转移性激素敏感性前列腺癌患者以1:1的比例随机分配接受达洛鲁胺(剂量为600mg[两片300mg片剂],每天两次)或匹配的安慰剂治疗,均与雄激素剥夺疗法和多西他赛联合使用。该研究的主要终点是总生存期。
该研究主要分析涉及1306名患者(达洛鲁胺组651名,安慰剂组655名);86.1%的患者在最初诊断时患有转移性疾病。在主要分析的数据截止日期(2021年10月25日),达洛鲁胺组的死亡风险显著低于安慰剂组32.5%(风险比为0.68;95%置信区间为0.57至0.80;P<0.001)。
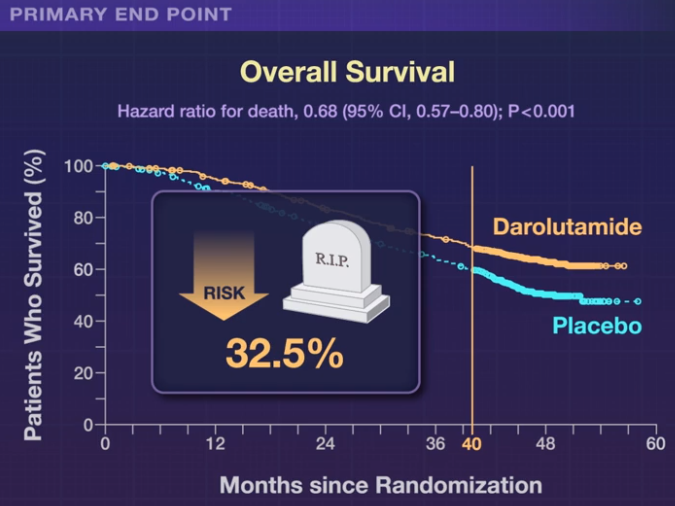
达洛鲁胺还与次要终点和预设亚组的持续获益相关。两组的不良事件相似,最常见的不良事件(发生在≥10%的患者中)的发生率在两组的重叠多西他赛治疗期间最高。达洛鲁胺组3级或4级不良事件的发生率为66.1%,安慰剂组为63.5%;中性粒细胞减少症是最常见的3级或4级不良事件(分别为33.7%和34.2%)。
由此可见,在这项涉及转移性激素敏感性前列腺癌患者的试验中,达洛鲁胺、雄激素剥夺疗法和多西他赛联合治疗的总生存期明显长于安慰剂加雄激素剥夺疗法和多西他赛,并且加用达洛鲁胺导致关键次要终点有所改善。两组的不良事件发生率相似。
原始出处:
Matthew R. Smith.et al.Darolutamide and Survival in Metastatic, Hormone-Sensitive Prostate Cancer.NEJM.2022.https://www.nejm.org/doi/full/10.1056/NEJMoa2119115
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#生存率#
38
#性激素#
53
#转移性#
31
#敏感性#
52