Nat Commun:抑制肿瘤细胞移动能防止癌症扩散
2018-11-30 佚名 中国生物技术网
对肿瘤细胞如何移动的新见解,将极大地有助于开发预防癌症扩散的新疗法。
美国明尼苏达大学的科学家们成功利用实验模型阻止了癌细胞扩散,即使这些癌细胞已经改变了它们的运动模式。
如果原发性肿瘤还未扩散,那么消灭癌症的概率就会大大提高。大约90%的癌症死亡病例都是由于癌细胞转移造成的,或者说是肿瘤侵袭附近的组织并且扩散到身体的其他部位。
一种能够阻止癌细胞移动的治疗方法将显着改善存活率,使医生拥有更多的时间处理原发性肿瘤。这项近日发表在《Nature Communications》上的研究或标志着这一成就向前迈出了一大步。
癌细胞的狡猾
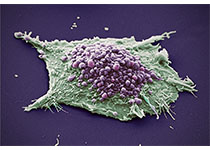
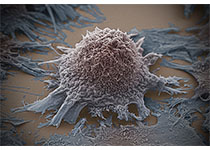
研究人员在实验室中建立了肿瘤环境,并观察乳腺癌细胞如何在环境中移动。他们利用药物扰乱被肿瘤细胞用作“马达”的机制,该机制为肿瘤细胞提供移动的动力。
令科学家们意外的是,这些细胞转换到一种完全不同的移动方式,使得它们像“渗出”的水滴一样。
研究通讯作者、明尼苏达大学生物医学工程系的助理教授Paolo P. Provenzano说:“癌细胞非常狡猾,我们并没有料到这些细胞会改变自己的移动方式。”
然而,同时以癌细胞移动的两种方式为靶标,研究人员们就能够阻止细胞的移动了。
Provenzano博士说:“就像是我们破坏了癌细胞的GPS,它们无法找到高速路入口,这些细胞就待在那里不能移动。”
癌症转移和细胞移动
癌症转移是一个复杂的过程,它分为几个阶段,每个阶段中,在癌症向下一阶段进展前都需要满足几个特定的条件。比如,在侵袭邻近组织期间,肿瘤细胞及其微环境或细胞外基质都经历显着的变化。由于被称为“接触指导”线索的复杂反馈,大多数细胞都具有穿过围绕它们细胞外基质的一些能力。
科学家们已经在各种环境中观察到了这种“指导”,例如伤口愈合以及器官的产生和再生。
Provenzano博士及其团队表示,“接触指导”还能帮助癌细胞感知并跟随肿瘤中的通路。他们把这种导向模式比作将入侵的癌细胞引导到“高速路”上。患有许多这些模式的肿瘤患者的存活率往往较低。
这项新研究的作者们指出,医学界仍然没有完全理解癌细胞是如何感知接触指导线索的。
工程化肿瘤微环境
为了研究肿瘤细胞如何识别并跟随这些通路,研究团队为此设计了2D微环境,模仿肿瘤中的指导线索模式。这种人工设计的环境显着地提升了研究速度。
该研究的第一作者Erdem D. Tabdanov博士解释说:“通过使用这些受控的网络微环境,我们能够在几个小时内测试数百个细胞移动事件,而如果使用肿瘤成像的方法,在同一时长内只能测试一到两次。”
接下来,研究团队想在其他种类的癌症上测试他们的方法,然后开始动物试验。如果结果良好,人体试验应该可以在几年内进行。研究人员还需要研究该方法的其他方面,例如对健康细胞的影响。
Provenzano博士说:“最终,我们希望找到方法抑制癌细胞移动,同时增强免疫细胞的移动以对抗癌症。”
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#抑制肿瘤#
48
#COMMUN#
41
#Nat#
33
#癌症扩散#
43
学习学习谢谢
75
#肿瘤细胞#
44