本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
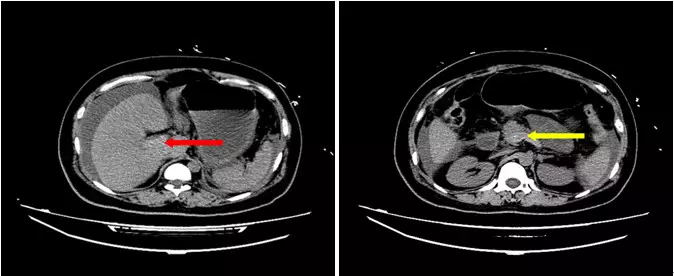
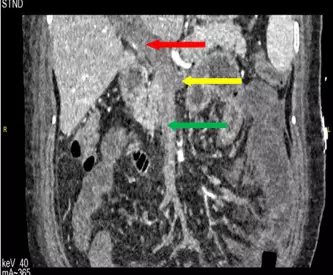

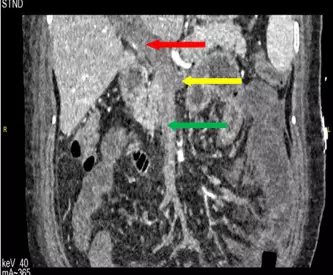
肠外瘘特点:消化道瘘包括肠外瘘、胆瘘与胰瘘,其中危害最大的是肠外瘘。消化道外瘘中的胆瘘漏出的是胆汁,胰瘘漏出的是胰液,肠瘘漏出的是肠液。胆汁本身无消化能力,胆汁漏出后对机体的影响主要是刺激作用。漏出的胰液如无激活,对机体的影响仅为水电解质丢失的影响。肠液因内含细菌和已激活的各种胰酶,其对机体的病理生理影响远较单纯胰液和胆汁的危害要大。 因肠液内含有大量细菌,肠液外溢后,可引起严重腹腔感染
如今,随着消化内镜技术的日益完善,临床上新的内镜下微创治疗方法层出不穷。然而,内镜下微创手术在给患者带来巨大益处的同时,也增加了各种医源性并发症,尤其是消化道穿孔及继发感染。 以往对无腹腔污染或有轻微污染的消化道穿孔,大多采用内镜下金属钛夹闭合术、专用工具缝合术、套扎技术和生物胶技术等方法进行治疗。但对于肠道准备欠佳且穿孔过大的病例,在行内镜下闭合穿孔时,可有肠腔内残存的粪便和含大量致病菌的肠液
背景:成功治疗腹腔感染,需要源头控制和抗生素的结合。但抗生素治疗的适当时间尚不清楚。 方法:研究人员招募了518例复杂腹腔感染患者,所有患者都在出现退烧、白细胞增多和肠梗阻2天后接受抗生素治疗,并且有适当的源控制。实验组接受固定抗生素治疗4±1天,对照组接受较长(最长达10天)的治疗期。根据治疗组情况,主要观察结果是手术部位感染,以及反复腹腔感染时或源控
减少抗生素治疗的持续时间是抗菌药物管理的一项基本措施。对于复杂的腹腔感染,抗生素治疗的最佳持续时间已经被广泛讨论,但对于ICU患者缺乏相关的数据。现有的指导方针没有提供相关的建议,只是建议决策过程应该基于临床医生的判断和实验室结果。


梅斯医学MedSci APP
医路相伴,成就大医
好文章学习了
0
辛苦了
61
学习了,谢谢分享
66
好文献学习了
64
ICU经常是大场面
71
#规培#
48
好文献学习了
40
谢谢分享
29
了解一下谢谢分享
36