Neurology:血液中神经丝蛋白预测亨廷顿病的局部萎缩!
2018-01-26 xing.T MedSci原创
由此可见,这些发现突出了NfL作为脑萎缩动态标志物的价值,并且为血浆NfL水平(候选的血液生物学标志物)与病理性神经元变化之间的较强相关性提供了进一步证据。
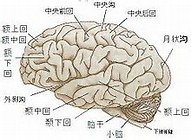
已有研究提出血浆中的神经丝(NfL)蛋白作为包括亨廷顿病(HD)在内的许多神经退行性疾病的预后生物标志物。近日,神经病学领域权威取杂志Neurology上发表了一篇研究文章,该研究旨在调查HD基因扩增携带者NfL相关的神经病理的区域分布。
研究人员对来自于国际多中心TRACK-HD研究中横断面(n=198)和纵向(n=177)数据评估了HD基因扩增携带者血浆中NfL与局部特异性萎缩之间的关联。使用基于体素的形态测量法,研究人员评估了基线NfL水平与基线灰质和白质体积之间的关联;以及随后3年HD基因扩增携带者灰质和白质的纵向变化。
在控制人口统计学指标后,在皮层和皮质下灰质以及白质内可见增加的NfL水平与减少的脑体积之间存在相关性。在控制疾病进展的已知预测因子(年龄和CAG重复长度)之后,相关性仅限于尾状核和壳核。纵向而言,在对疾病进展的其他预测因子进行校正之前和之后,NfL可预测随后的枕骨灰质萎缩和广泛的白质减少。
由此可见,这些发现突出了NfL作为脑萎缩动态标志物的价值,并且为血浆NfL水平(候选的血液生物学标志物)与病理性神经元变化之间的较强相关性提供了进一步证据。
原始出处:
Eileanoir B. Johnson,et al.Neurofilament light protein in blood predicts regional atrophy in Huntington disease.Neurology. 2018.https://doi.org/10.1212/WNL.0000000000005005
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#萎缩#
33
#神经丝蛋白#
34
#神经丝#
37
#Neurol#
31
#亨廷顿病#
31
#局部#
39
#亨廷顿#
30
谢谢
55
学习谢谢分享
63