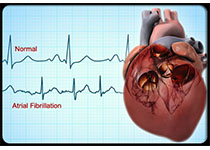
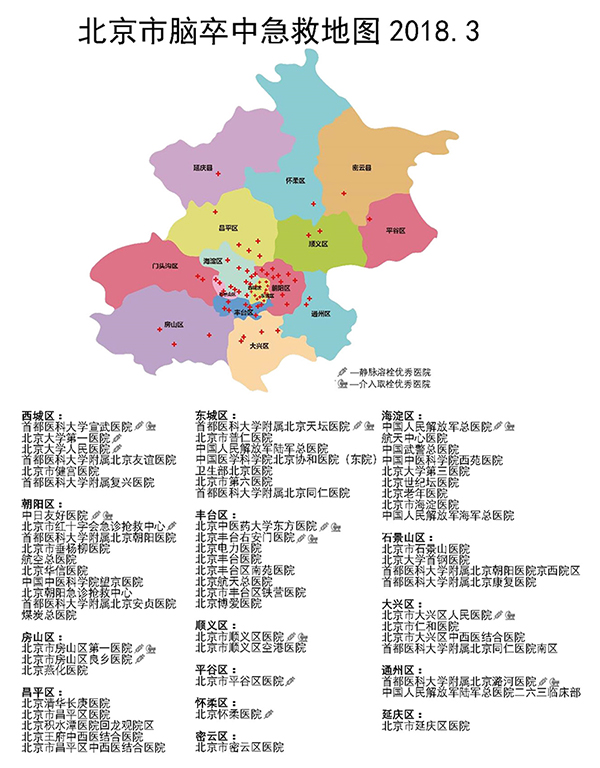
Neurology:卒中后新发房颤是卒中的因还是果?
2018-04-10 杨中华 脑血管病及重症文献导读
心脏疾病对脑有直接影响,比如房颤会引起脑栓塞。脑部疾病对心脏的影响是什么?比如缺血性卒中。有趣的是,岛叶皮质损害者更容易新诊断缺血性卒中后房颤(AF)。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#卒中后#
35
#Neurol#
51
学习学习学习
98
#新发房颤#
47
学习
78
学习了受益匪浅
85
好文献.学习学习好文献.学习学习
71
学习一下谢谢
67
卒中虽然是临床上常见病,溶栓,取栓等血管内治疗也很成熟,但是仍然有很多未知问题有待认知!
33
呃?
38