Hepatol:完全生化缓解与瞬时弹性成像可检测自身免疫性肝炎患者疾病进展
2017-11-30 MedSci MedSci原创
本研究表明,完全生化缓解是AIH预后良好的一个可靠预测因子,可预测患者肝纤维化缓解。
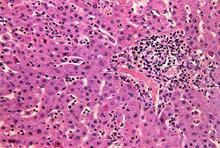
研究背景:在治疗的自身免疫性肝炎(AIH)患者中,会发生肝纤维化缓解,但也可能发生纤维化进展。在AIH中,有必要发现新的非侵入性替代标记,以便更好地指导免疫抑制治疗。本研究旨在评估完全生化缓解(转氨酶和IgG正常)对肝组织病理学和纤维化发展的影响,以及重复瞬时弹性成像(TE)测定对监测AIH疾病进展的价值。
研究方法:对60例AIH患者的131例肝组织和125例AIH患者、130例原发性胆汁性胆管炎(PBC)患者、100例原发性硬化性胆管炎(PSC)患者的900多次瞬时弹性成像进行评估。至少间隔12个月,进行再次瞬时弹性成像检测。AIH患者在进行第一次瞬时弹性成像检测后,至少进行6个月的治疗。
研究结果:相比PBC和PSC患者,AIH患者肝硬度显著下降(-6.2%/年, CI95%: -12%.6 to -0.2%, p=0.04)。基线时,肝纤维化程度严重的患者,肝硬度下降最高。(F4: -11.7%/年, -19% to -3.5%, p=0.006)。完全生化缓解与LS的回归密切相关("缓解": -7.5%/年 vs. "未缓解": +1.7%/年, p<0.001)。相似的是,完全生化缓解能够预测低组织学疾病活动,是唯一能够独立预测肝组织纤维化缓解的因素 (RR 3.66, CI95% 1.54-10.2, p=0.001)。仍然保持完全生化缓解的3期/4期肝纤维化患者,在组织学随访过程中,肝纤维化分期显著下降(3.7±0.5到1.8±1.7, p=0.007)。
研究结论:本研究表明,完全生化缓解是AIH预后良好的一个可靠预测因子,可预测患者肝纤维化缓解。
原始出处
Hartl J, Ehlken H, Sebode M, et al. Usefulness of biochemical remission and transient elastography in monitoring disease course in autoimmune hepatitis. J Hepatol, 2017, Nov 24. pii: S0168-8278(17)32445-5. doi10.1016/j.jhep.2017.11.020.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#肝炎患者#
33
#疾病进展#
31
#生化缓解#
25
#瞬时弹性成像#
0
#弹性成像#
0
#EPA#
22