Br J Cancer:CirCe01随机试验分析基于循环肿瘤细胞的化疗监测策略对于转移性乳腺癌患者的临床实用性
2021-01-25 xiaozeng MedSci原创
转移性乳腺癌(MBC)是全球女性癌症死亡的主要原因之一。
转移性乳腺癌(MBC)是全球女性癌症死亡的主要原因之一。如高级别乳腺癌共识会议上所述,MBC是一种无法治愈的但可进行治疗的疾病,在HER2阳性(HER2+)以及雌激素受体阳性(ER+)亚组中,患者的平均总生存期>5年。虽然患者在接受一线化疗后可能会伴随着化疗耐药性的产生。
尽管目前艾日布林(eribulin)用作二线或三线化疗药物已显示出了对总体生存率的统计学上的显著改善,但随后后期化疗的生存获益仍存在争论。目前尚无相关临床特征或临床标志物可用于确定晚期化疗患者是否受益。
循环肿瘤细胞(CTC)是一种可以在外周血中检测到的稀有肿瘤细胞。早在2004年发表一项关于177个MBC患者的研究就提出了区分MBC患者的界别。基于相关的临床有效性数据。CTC计数的早期变化已被确认为是患者的一个预后标志物,既往的多项研究也证实了CTC计数的有效性。
CirCe01试验设计
在该研究中,研究人员报告了CirCe01试验的结果,这是一项基于CTC的前瞻性试验,旨在评估基于CTC的监测在三线化疗(LC)后对MBC患者的临床实用性。
CirCe01是一项前瞻性、多中心的随机试验(NCT01349842),主要纳入了两次系统性LC后CTC监测≥5 CTC/7.5 mL的MBC患者。患者被随机分为CTC驱动组和标准组。在CTC组中,在每个LC疗程的第一个周期评估CTC计数的变化。CTC水平预测的肿瘤早期进展的患者将改变随后的LC治疗策略。
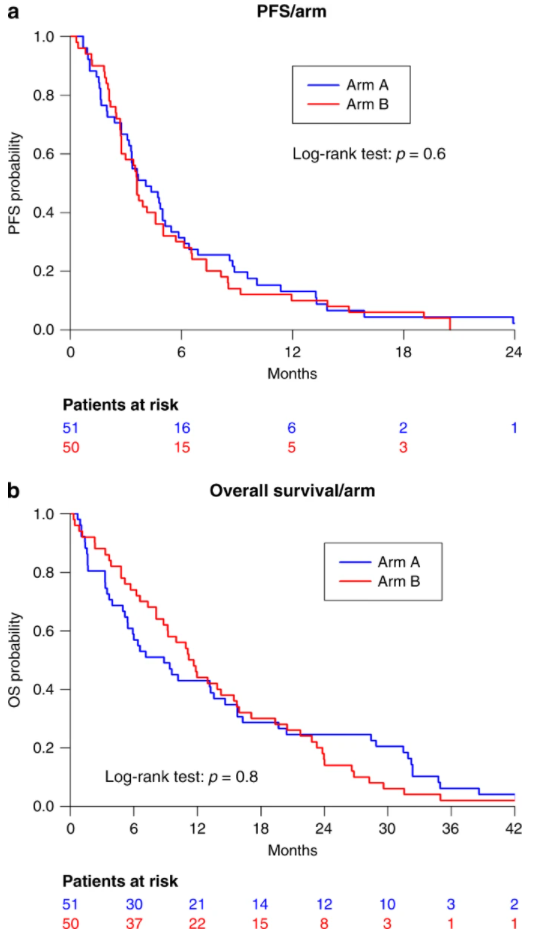
患者的生存曲线
在总的204名患者中,有101名患者中观察到≥5 CTC/7.5 mL。在CTC组(N=51)中,分别有43(83%)和18(44%)名患者在三线、四线治疗中完成了CTC的监测,其中分别有18(42%)和11(61%)名患者对CTC无响应。在这些患者中,分别有13(72%)和5(46%)名患者出现了疾病的早期进展并切换至下一次的LC治疗。
进一步研究显示,两组的总体生存率无显著性差异。亚组分析显示,无CTC反应且转用化疗的患者相比于未接受化疗的患者具有更长的生存期。
总而言之,该研究旨在评估重复CTC检测的化疗方案是否可以提供显著的生存获益。由于应计性和药物依从性等问题,该试验未能证明CTC监测的临床效用。
原始出处:
Cabel, L., Berger, F., Cottu, P. et al. Clinical utility of circulating tumour cell-based monitoring of late-line chemotherapy for metastatic breast cancer: the randomised CirCe01 trial. Br J Cancer (21 January 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#实用性#
41
#监测策略#
32
#肿瘤细胞#
41
#转移性#
48
#随机试验#
46
#乳腺癌患者#
34
#循环肿瘤细胞#
51
高质量研究,读起来真爽,谢谢梅斯
46