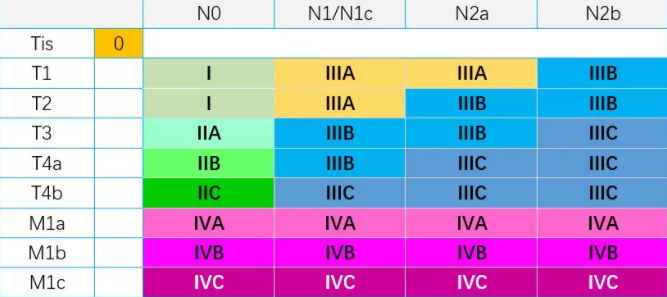
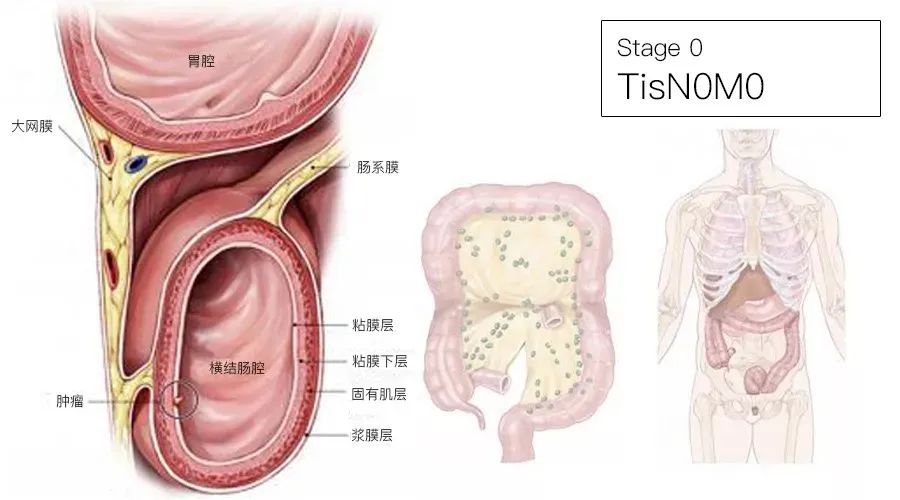
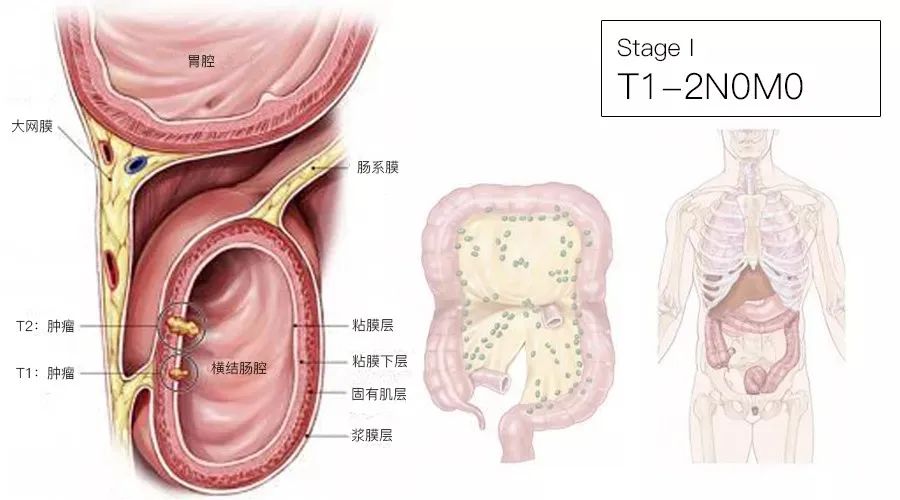
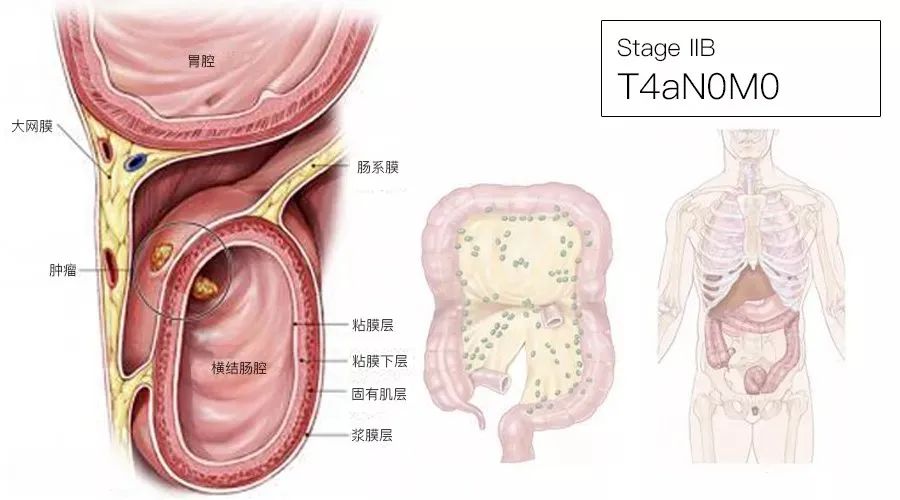
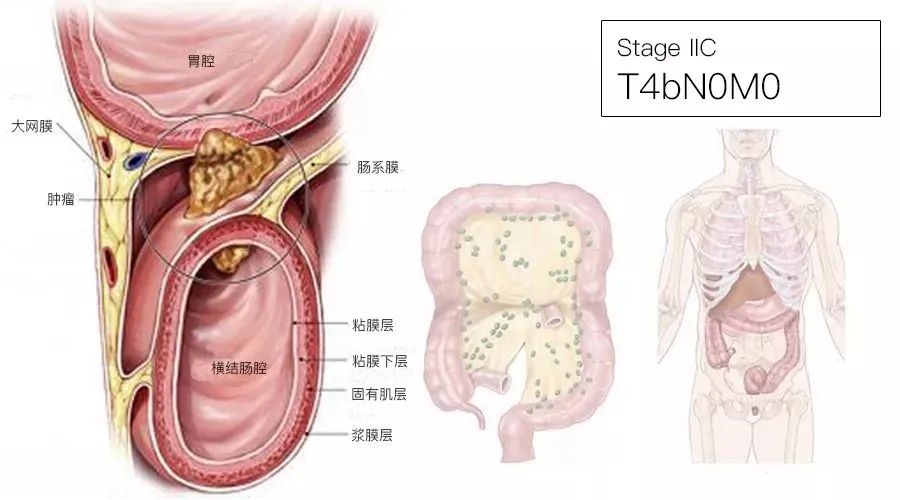
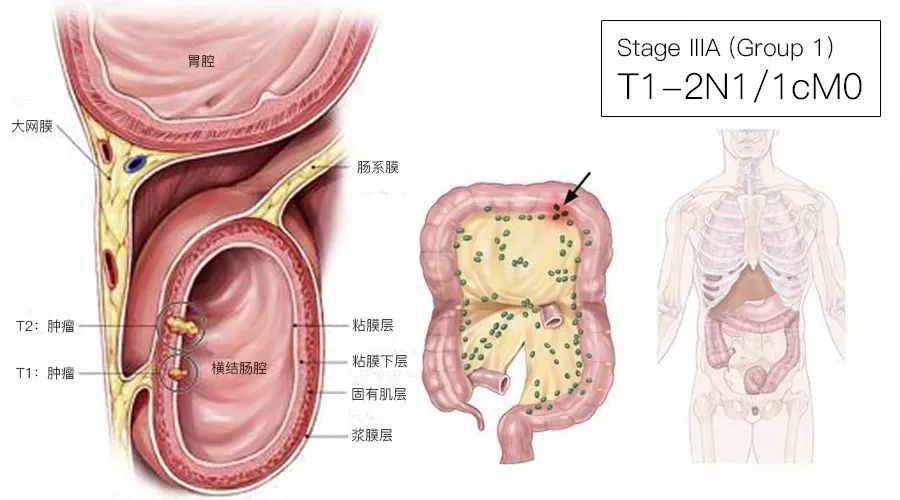
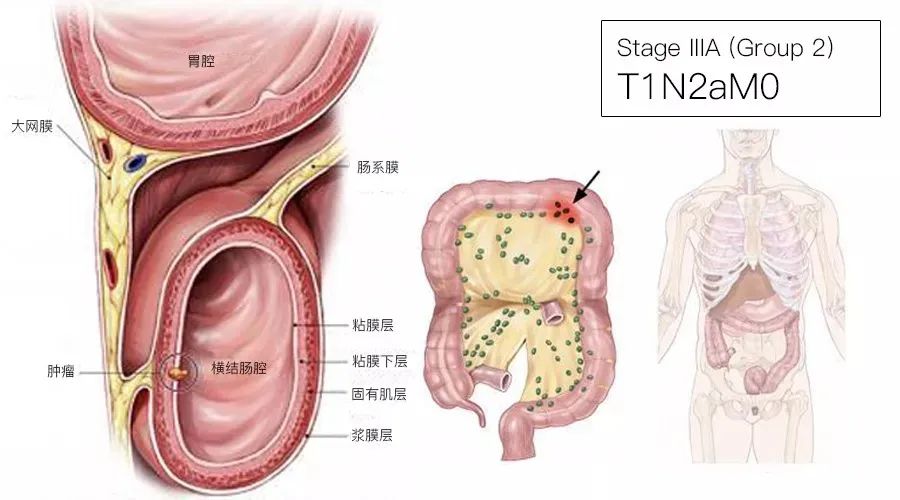
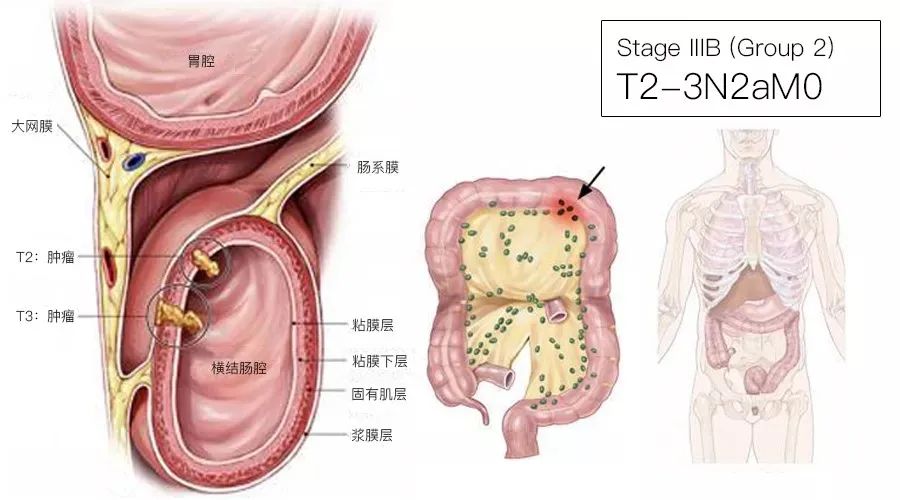
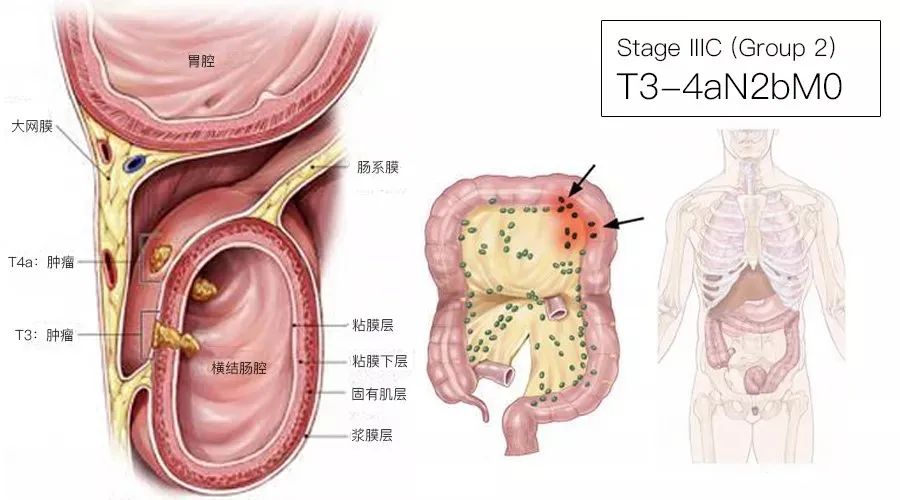
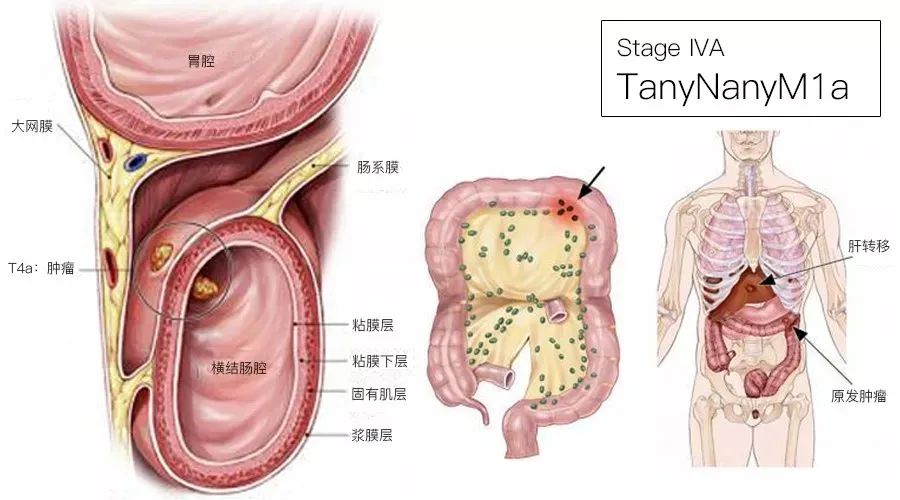
导读: 肿瘤分期是临床诊断和治疗的依据,目前常用的方法为TNM分期。第八版的更新再次强调了结直肠癌生物学信息和基因检测的重要性。 一、T、N、M定义 T:代表原发肿瘤的情况 Tx:原发肿瘤无法评价 T0:无原发肿瘤证据 Tis:原位癌,黏膜内癌(肿瘤侵犯黏膜固有层但未突破黏膜肌层) T1:肿瘤侵犯黏膜下层(肿瘤侵犯黏膜下层但未累及固有肌层) T2:肿瘤侵犯固有肌层 T3:肿瘤穿透固有肌层到达结直肠旁组织 T4:肿瘤侵犯腹膜脏层或侵犯或粘连于临近器官或结构 T4a:肿瘤穿透脏层腹膜(包括肉眼可见的肿瘤部位肠穿孔,以及肿瘤透过炎症区域持续浸润到达脏层腹膜表面) T4b:肿瘤直接侵犯或附着于邻近器官或结构 N:代表区域淋巴结 Nx:区域淋巴结无法评价 N0:无区域淋巴结转移 N1:有1-3枚区域淋巴结转移(淋巴结中的肿瘤直径≥0.2mm),或无区域淋巴结转移、但存在任意数目的肿瘤结节(tumor deposit,TD) N1a:有1枚区域淋巴结转移 N1b:有2-3枚区域淋巴结转移 N1c:无区域淋巴结转移,但浆膜下、肠系膜内、或无腹膜覆盖的结肠/直肠周围组织内有肿瘤结节 N2:有4枚及以上区域淋巴结转移 N2a:有4-6枚区域淋巴结转移 N2b:有≥7枚区域淋巴结转移 M:代表远处转移,表示肿瘤扩散到其他部位 Mx:远处转移无法评价 M0:影像学检查无远处转移,即远隔部位和器官无转移肿瘤存在的证据(该分类不应该由病理医师来判定) M1:存在一个或多个远隔部位、器官或腹膜的转移 M1a:远处转移局限于单个远离部位或器官,但没有腹膜转移 M1b:远处转移分布于两个及以上的远离部位或器官,无腹膜转移M1c:腹膜转移,伴或不伴有其他部位或器官转移 M1C:腹膜转移有或没有其他器官转移 1、Tis 包括肿瘤细胞局限于腺体基底膜(上皮内)或黏膜固有层(黏膜内),未穿过黏膜肌层到达黏膜下层。 2、T4b T4b的直接侵犯包括穿透浆膜侵犯其他肠段,并得到镜下诊断的证实(如盲肠癌侵犯乙状结肠),或者位于腹膜后或腹膜下肠管的肿瘤,穿破肠壁固有基层后直接侵犯其他的脏器或结构,例如降结肠后壁的肿瘤侵犯左肾或侧腹壁,或者中下段直肠癌侵犯前列腺、精囊腺、宫颈或阴道。 肉眼观察到肿瘤与邻近器官或结构粘连分期为cT4b,若显微镜下该粘连处未见肿瘤存在分期为pT3。 3、TD 淋巴结有转移时,肿瘤种植的结节数目不纳入淋巴结计数,单独列出。 4、V和L亚分期 用于表明是否存在血管和淋巴(LV1),而PN1则用以表示神经浸润。 5、前缀 cTNM代表临床分期,pTNM代表病理分期。两者都用来帮助制定治疗计划。由于病理分期是由术中取得的肿瘤组织确定的,因此病理分期可以比临床分期更好的指导手术后下一步的治疗方案(随访或化疗或放化疗等),也能更准确的预测病人的预后。 前缀y用于接受新辅助治疗后的肿瘤分期(如ypTNM),病理学完全缓解的患者分期为ypT0N0cM0,可能类似于0期或1期。前缀r用于经治疗获得一段无瘤间期后复发的患者(rTNM)。 二、结直肠癌分期图谱 三、8th VS 7th 1、AJCC第8版结直肠癌分期 UICC/AJCC颁布了第 8 版结直肠癌 TNM分期系统。总体看本次更新变化不大,但更新特色是推动了临床肿瘤学预后(prognostic)和预测(predictive)评价体系的完善和提高。 2、TD TD(tumor deposit):特指存在于原发肿瘤淋巴引流区域内(结肠系膜和直肠系膜的脂肪组织内)的孤立肿瘤结节。第八版分期系统认为TD是较差的预后因素,并继续把TD划归为N1c;TD不改变T分期;如无区域淋巴结转移,TD会改变N分期(N0→N1c );如有区域淋巴结转移,TD数目无需计算到阳性淋巴结数量。 3、M 分期 M1a:转移灶局限在一个器官或部位; 4、预后风险评价模型 AJCC精准医学核心组对现有结直肠癌预后风险评估工具进行了遴选,最终在29个评估工具中挑选了3项完全符合AJCC质量控制标准并给予推荐:Mayo(III期结肠癌复发及总生存);MSKCC(结肠癌术后生存预测);Euro(局部进展期直肠癌复发、转移、总生存)。





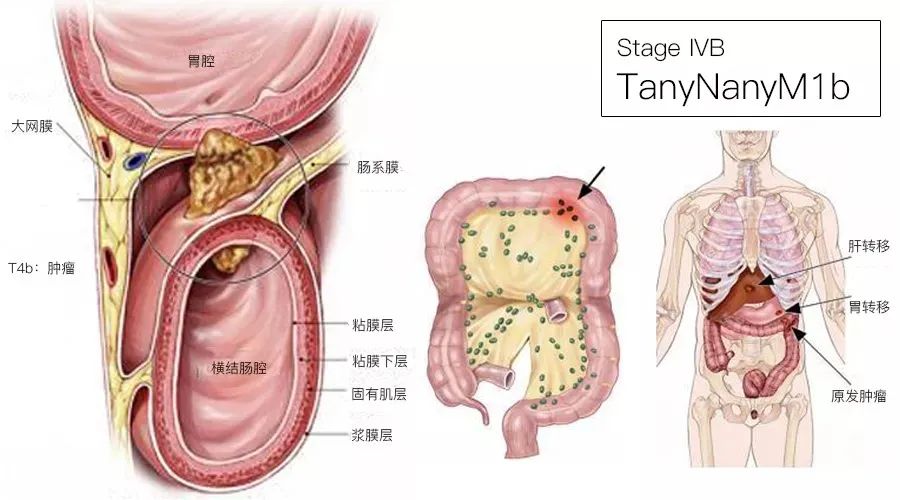
M1b:转移灶超出一个器官或部位,但没有腹膜转移;
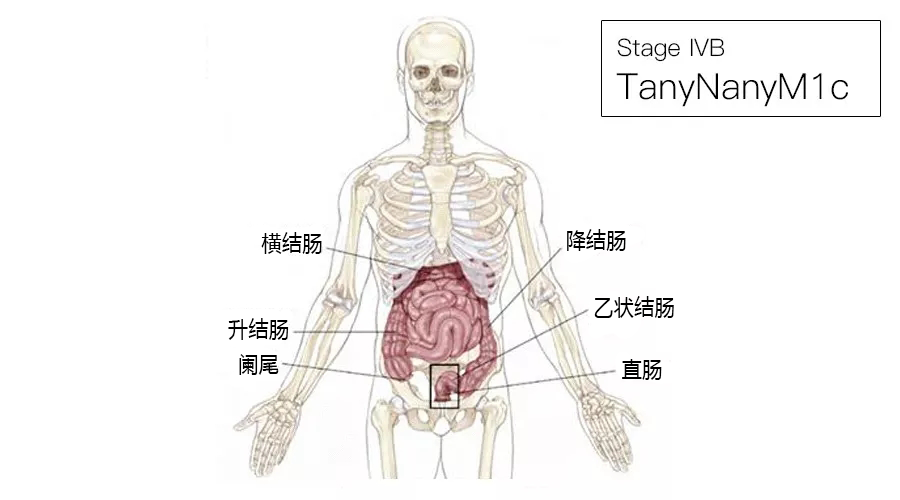
M1c:结直肠癌的腹膜转移,无论是否合并其他器官部位的转移(新增M1c仅见于1~4%的结直肠癌患者,但其预后较M1a和M1b更差)。
参考资料:AJCC第8版结直肠癌TNM分期图谱
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












👍
42
不错
40
#TNM#
61
#TNM分期#
62
#结直肠#
43
学习了
55