耐药性晚期癌症如何治疗?靶向耐药途径IRS1/2和STAT3的NT219即将进行I/II期临床试验
2020-05-24 Allan MedSci原创
Kitov是一家临床阶段的生物技术公司,致力于克服肿瘤的免疫逃逸和耐药性。
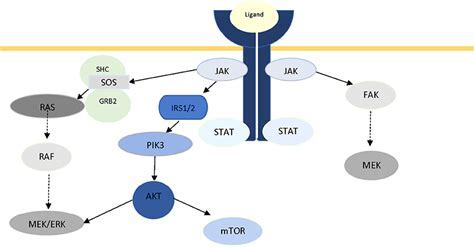
Kitov是一家临床阶段的生物技术公司,致力于克服肿瘤的免疫逃逸和耐药性,Kitov近日宣布,美国FDA已接受其研究性药物(IND)申请,允许开展NT219治疗耐药性晚期癌症的I/II期临床试验。NT219是一种针对晚期癌症耐药性的新型药物,是靶向耐药途径IRS1/2和STAT3的小分子。这项研究将评估NT219作为单药疗法或与利妥昔单抗(抗EGFR单克隆抗体)联合治疗复发或转移性实体瘤(包括头颈癌和鳞状细胞癌)的有效性和安全性。
Kitov首席医学官Bertrand Liang博士说:“基于NT219的临床前数据,我们认为该候选药物有望成为治疗多种耐药性癌症有效疗法”。开放标签的I期临床试验的主要目标是评估安全性和药代动力学,确定在II期临床试验中合适的剂量以及确定NT219的初步疗效。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#I期临床#
34
#I期临床试验#
22
#II期临床试验#
35
#NT219#
28
#STAT3#
44
#II期临床#
28