JCEM:益生元改善接受胃旁路术的绝经后妇女钙吸收水平
2021-12-11 MedSci原创 MedSci原创
在FCA或促钙激素的变化方面没有观察到组间差异,但较宽的置信区间表明SCF的可变效应可能是由于肠道微生物组改变的程度所致。每日摄入SCF具有较好的耐受性,但需要更大型和更长期的研究进一步验证。
Roux-en-Y胃旁路术(RYGB)对骨骼的不利影响部分是由肠道钙吸收下降所引起的。益生元,如可溶性玉米纤维(SCF),可增加健康个体的结肠钙吸收水平。
近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,研究人员旨在评估SCF对RYGB后人群的钙吸收分数(FCA)、生化参数和粪便微生物组的影响。
这项随机、双盲、安慰剂对照试验是在20名平均5年前接受RYGB的绝经后妇女中进行的。该研究的干预措施为口服20g/天的SCF或麦芽糊精安慰剂,口服2个月疗程。该研究的主要结局为FCA绝对变化的组间差异,是采用金标准双稳定同位素方法测量的。其他指标包括耐受性、依从性、血清促钙激素和骨转换标志物,以及通过16SrRNA基因测序的粪便微生物组成。
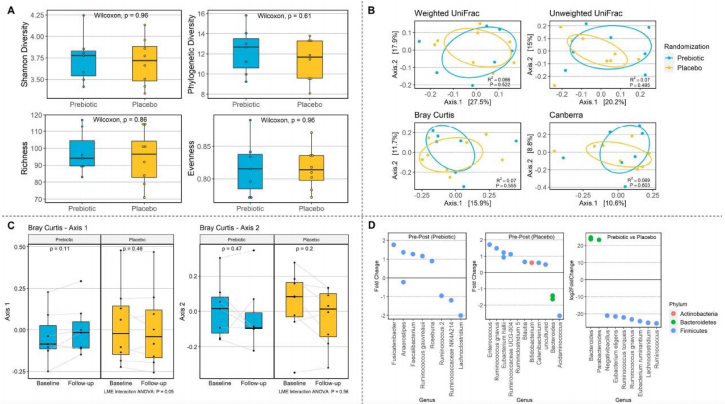
基线时的平均FCA±SD较低,为5.5±5.1%。将SCF与安慰剂进行比较,FCA的平均(95%CI)变化(+3.4[-6.7,+13.6]%)、促钙激素或骨转换标志物均无组间差异。与安慰剂相比,SCF组的FCA变化变化更大(SD为13.4%与7.0%)。SCF治疗后微生物组成变化较大个体FCA增加程度较大(r2=0.72,p=0.05)。SCF治疗依从性高,组间胃肠道症状相似。
由此可见,在FCA或促钙激素的变化方面没有观察到组间差异,但较宽的置信区间表明SCF的可变效应可能是由于肠道微生物组改变的程度所致。每日摄入SCF具有较好的耐受性,但需要更大型和更长期的研究进一步验证。
原始出处:
Karin C Wu.et al.Prebiotic to Improve Calcium Absorption in Postmenopausal Women After Gastric Bypass: A Randomized Controlled Trial.JCEM.2021.https://academic.oup.com/jcem/advance-article/doi/10.1210/clinem/dgab883/6458466
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#胃旁路术#
0
#胃旁路#
48
#JCE#
38
#JCEM#
34
学习了
59
#绝经#
39
#绝经后妇女#
43
#益生元#
34
#绝经后#
33