Clin Microbiol Infect:铜绿假单胞菌在慢性阻塞性肺疾病患者中的持久性和遗传适应性
2022-03-12 从医路漫漫 MedSci原创
铜绿假单胞菌是慢性阻塞性肺疾病(COPD)患者细菌感染的常见原因,可从4%-15%的成人COPD患者的痰标本中分离到铜绿假单胞菌。
背景:铜绿假单胞菌是慢性阻塞性肺疾病(COPD)患者细菌感染的常见原因,可从4%-15%的成人COPD患者的痰标本中分离到铜绿假单胞菌。可以从呼吸道培养出铜绿假单胞菌的COPD患者病情恶化和死亡的风险显著增加,这更可能出现在最近接受抗生素治疗的患者和需要机械通气的患者中。在大多数情况下,一种菌株的携带时间很短,然而一小部分患者可能会持续在铜绿假单胞菌中定居数年。导致铜绿假单胞菌致病性的主要因素是III型分泌相关的细胞毒性和产生群体感应调节的毒力因子,如绿青素、碱性蛋白酶和弹性蛋白酶。一些保守的微生物结构通过细胞表面和内体Toll样受体(TLR)激活宿主免疫反应,如TLR4和TLR5。我们的目的是阐明IL-17在发病机制中的作用。
方法:我们检测了IL-23/IL-17A在COPD稳定期患者(n=33)和COPD急性加重期合并铜绿假单胞菌感染患者(n=34)中的表达及其影响。以慢性阻塞性肺疾病(COPD)小鼠模型(C57BL/6)为模型,应用IL-17A中和抗体或重组IL-17A,研究IL-17A在宿主抗铜绿假单胞菌感染炎症反应中的作用。
结果:我们发现铜绿假单胞菌感染增加了COPD患者和COPD小鼠模型肺中IL-23/17A信号。当针对IL-17A的中和抗体处理COPD小鼠模型时,铜绿假单胞菌诱导的中性粒细胞浸润和肺内细菌负荷比未治疗的小鼠明显减少。中和抗体对肺功能也有改善作用。IL-17A信号传导阻断可显著降低促炎细胞因子IL-1b、IL-1 8、T N F-a、C X C L 1、C X C L 1 5a和d M M P-9的表达,增加抗炎细胞因子IL 10和IL 1ra的表达。小鼠重组IL-17A的应用加剧了铜绿假单胞菌介导的炎症反应和COPD小鼠模型的肺功能障碍。细胞因子蛋白芯片显示视黄醇结合蛋白4(RBP4)的表达受IL-17A下调,外源性RBP4重组蛋白可减轻铜绿假单胞菌诱导的气道功能障碍。
图1 稳定期COPD(COPD,n=33)和铜绿假单胞菌感染COPD(PA-COPD,n=34)患者的中性粒细胞、肺功能和BALF IL-23/IL-17A水平。PA-COPD患者BALF中性粒细胞绝对数和百分比较高,而血液(A、B)无明显变化。比较COPD和PA-COPD患者的用力呼气容积(C)、呼气流量(D)和强迫振荡试验(E)。PA-COPD(F)患者IL-23、IL-17A水平明显升高。数据以平均值±标准差表示。*P<0.05,**P<0.01,ns,无显著性。相关分析显示两种细胞因子(G)呈显著正相关,进一步回归分析提示IL-23可能是导致IL-17A(H)升高的重要因素。BALF中IL-17A水平与中性粒细胞绝对数(I)呈显著正相关。肺活量测定结果(FEV1.0%预测值(J)、FEV1.0/FVC%(K)、MMEF(L))与IL-17A水平呈负相关。BALF,支气管肺泡灌洗液;COPD,慢性阻塞性肺疾病;IL,白细胞介素;FEV1.0,一秒用力呼气量;FVC,用力肺活量;MMEF,最大呼吸中段流量。
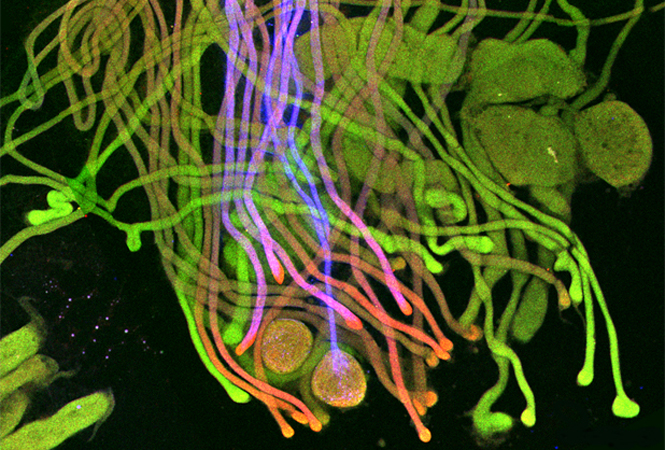
图2 铜绿假单胞菌感染增加了COPD小鼠模型肺中IL-23/IL-17轴信号。C57BL/6小鼠暴露于臭氧中,每周2次,连续6周建立COPD模型,然后经支气管内接种无菌琼脂微球(con-COPD)或1.0×105CFU琼脂包裹的铜绿假单胞菌(PA-COPD)。接种后1d取肺切片,Masson三色染色检测组织纤维化(A,上排),PAS定量糖原[(A,下排)]。气道周围的蓝色区域为胶原沉积(用黑色箭头表示),气管腔内的紫色区域表示粘液分泌和杯状细胞增生(用蓝色箭头表示)。内部比例尺=100 mm。采用实时荧光定量PCR、半定量RT-PCR和Western-blot检测肺组织中IL-23及其受体(B)和IL-17A及其受体(C)的表达。B-肌动蛋白作为负荷控制。数据以平均值±标准差(n=5)表示。**P<0.01。肺组织进行免疫荧光分析(D),切片用抗IL-17RA(红色)、抗Ly6G(绿色)和DAPI(蓝色)进行细胞核染色。内部比例尺=100 mm。进行了两个独立的实验。相关分析显示Ly6G+IL-17RA+细胞数与肺活量测定结果(E)呈显著负相关。COPD,慢性阻塞性肺疾病;CFU,集落形成单位;IL,白细胞介素;FVC,用力肺活量;FEV50,快速呼气前50ms容量过期。
图3|IL-17A信号促进铜绿假单胞菌感染COPD小鼠模型的肺损伤。COPD小鼠模型在接种1.0×105CFU铜绿假单胞菌前4h腹腔注射IL17A中和抗体(2 mg/kg)或重组IL-17A(1.6 mg/kg)。以小鼠IgG和BSA为对照。接种后1d(A、D)取肺组织行苏木精-伊红染色。每张肺显微照片中的数字是指定的浸润评分。MPO单位测定(B,E),细菌平板计数(C,F)。肺切片用抗IL-17RA(红色)、抗Ly6G(绿色)和DAPI(蓝色)免疫荧光染色细胞核(G)。内部比例尺=100 mm。比较不同组间肺活量测定结果,包括FVC、FEV50、MMEF、FEF50和FEF75。数据以平均值±标准差(n=5)表示。*P<0.05,**P<0.01,ns,无显著性。COPD,慢性阻塞性肺疾病;MPO,髓过氧化物酶;CFU,集落形成单位;BSA,牛血清白蛋白;IL,白细胞介素;FVC,用力肺活量;FEV50,快速呼气前50ms内呼气容积消失;MMEF,最大呼气中期流速;FEF50,用力呼气流速为50%FVC;FEF75,用力呼气流速为75%FVC。
结论:联合应用IL-17A中和抗体和环丙沙星减轻COPD小鼠模型接种铜绿假单胞菌后的气道炎症和通气。提示IL-17在慢性阻塞性肺疾病急性加重期铜绿假单胞菌气道感染的发病机制中起重要作用。靶向IL-17A是控制COPD患者铜绿假单胞菌感染结局的潜在治疗策略。、
原文出处:Ding F, Han L, Fu Q,et al.Pseudomonas aeruginosaIL-17 Aggravates Airway Infection in Acute Exacerbations of Chronic Obstructive Pulmonary Disease.Front Immunol 2021;12
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言





.jpg)





#Bio#
31
#Biol#
52
#阻塞#
49
#疾病患者#
36
#CRO#
37
#Micro#
30
#适应性#
31