Science:肠道微生物竟然影响癌症免疫治疗效果?!
2015-11-10 佚名 生物谷
检查点抑制剂是能够唤醒免疫系统抵抗肿瘤的新型药物,对癌症的治疗具有显著的疗效。然而一些临床结果表明该类药物对一部分病人并没有效果。最近两篇研究文章对此内在的机理进行了阐释。作者们认为这部分病人体内的微生物种群存在异常,因而不能正常地产生免疫反应。 这两项研究第一次将免疫检查点抑制剂与肠道的菌群联系起来。正常情况下,免疫细胞表面的一些受体能够限制其对自体组织进行杀伤。然而肿瘤组织同样能够激活

检查点抑制剂是能够唤醒免疫系统抵抗肿瘤的新型药物,对癌症的治疗具有显著的疗效。然而一些临床结果表明该类药物对一部分病人并没有效果。最近两篇研究文章对此内在的机理进行了阐释。作者们认为这部分病人体内的微生物种群存在异常,因而不能正常地产生免疫反应。
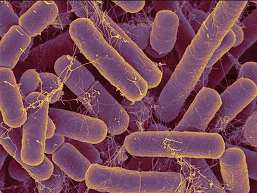
这两项研究第一次将免疫检查点抑制剂与肠道的菌群联系起来。正常情况下,免疫细胞表面的一些受体能够限制其对自体组织进行杀伤。然而肿瘤组织同样能够激活这些受体,导致特异性的免疫细胞无法对其进行识别与杀伤。像ipilimumab等免疫检查点抑制剂则能够通过阻止肿瘤细胞对这些受体的激活而维持免疫细胞的活性。
这项新的研究能够改变医生用药的方式。“这两篇文章证明了微生物能够影响治疗效果”,来自NIH的过敏与传染病研究所的免疫学家Yasmine Belkaid说到。过去研究者们经常专注于寻找患者基因组中的的突变,并以此解释为何免疫检查点抑制剂药物治疗效果存在个体差异。而如今的这两篇研究指出除基因组之外,微生物可能也有同样的影响。
免疫检查点抑制剂能够缩小肿瘤病延长患者的寿命。然而并不是所有患者都能够达到此效果。比如,仅有20%的黑色素瘤患者经过ipilimumab治疗后获得了寿命的延长,而研究者们此前也一直不清楚这一类群与那不幸的80%患者有何不同。
这类药物的一项副作用使得来自法国的癌症免疫学家Laurence Zitvogel产生了兴趣。Ipilimumab经常能够引发溃疡(一类肠道炎症),并引起肠道内一部分细菌的死亡。这一副作用暗示Ipilimumab的药效可能与肠道的微生物有很大关系。之后的实验证明了免疫检查点抑制剂对于患有癌症且肠道微生物缺失小鼠治疗效果并不明显。
之后,Zitvogel等人认为是肠道内某一特定类型的细菌参与了微生物的抗肿瘤效应。为了验证这一猜想,作者们将特定的微生物定殖到无菌小鼠肠道内部。结果显示,肠道菌的再生能够增强免疫检查点抑制剂的疗效。
同时,来自芝加哥大学的免疫学家Thomas Gajewski得到了相似的结论。他发现两株来源不同的同一品系小鼠产生了不同的表型:来自于Jackson Laboratory的小鼠体内黑色素瘤的生长速度明显慢于来自Taconic Farms的小鼠。额将它们共同饲养之后这一差异便消失了。由此,他们认为是肠道呢IDE微生物种群的差异影响了肿瘤的生长。
之后,作者们开始分析是何种微生物真正影响了小鼠抗肿瘤的结果。他们鉴定出了Bifidobacterium是一类关键的细菌类型。以上两个研究组的结果都同时发表在最近一期的《Science》杂志上。
两个研究组所鉴定得到的关键微生物类型并不相同,然而佛罗里达大学医学院的微生物免疫学家Christian Jobin却并不在意。他认为其内在的本质依然是相同的。
这项新发现“打开了癌症治疗的新大门,也许未来人们可以通饲喂特定的菌株达到提高癌症治疗效果的目的”。
原文出处:
Ayelet Sivan,Leticia Corrales,et al.Commensal Bifidobacterium promotes antitumor immunity and facilitates anti–PD-L1 efficacy.science.2015
Marie Vétizou,Jonathan M. Pitt,et al. Anticancer immunotherapy by CTLA-4 blockade relies on the gut microbiota.science.2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#微生物#
40
赞
109
#治疗效果#
0
受教了!
118
#SCIE#
27