JACC:肺动脉高压患者初始三联口服治疗可能改善长期预后
2021-10-03 刘少飞 MedSci原创
肺动脉高压 (PAH) 是一种不断发展的疾病,许多病理生理机制促成了其进展。在鉴定出的那些中,前列环素、内皮素和一氧化氮途径可以成为药物治疗的目标。针对多种途径的联合治疗是 PAH 管理的重要组成部分

肺动脉高压 (PAH) 是一种不断发展的疾病,许多病理生理机制促成了其进展。在鉴定出的那些中,前列环素、内皮素和一氧化氮途径可以成为药物治疗的目标。针对多种途径的联合治疗是 PAH 管理的重要组成部分。与初始单药治疗相比,内皮素受体拮抗剂 (ERA) 和 5 型磷酸二酯酶抑制剂 (PDE5i) 的初始双重治疗可延迟 PAH 进展,推荐用于新诊断的 PAH 患者的 1 年死亡率中低风险。
接受双重口服治疗(包括初始双重治疗)的患者继续经历 PAH 进展,这为更强化治疗提供了依据。不受控制的回顾性分析表明,与基线相比,包括胃肠外前列环素类似物在内的初始三联疗法改善了新诊断为重度 PAH 的患者的血流动力学状态和功能能力,并具有出色的生存率。此外,在 GRIPHON(Selexipag [ACT-293987] in Pulmonary Arterial Hypertension)随机对照试验中,对基线时接受双重口服治疗的患者服用 selexipag,一种口服选择性前列环素受体(IP 受体)激动剂,降低了复合发病率和死亡率终点事件。然而,没有数据比较 PAH 患者的初始三联疗法与初始双重疗法。
TRITON(初始三联疗法与初始双重口服联合治疗在新诊断肺动脉高压患者中的疗效和安全性)评估了初始口服马西替坦、他达拉非和司来帕格三联疗法与初始双重口服马西替坦和他达拉非在新诊断、未接受过治疗的 PAH 患者中的应用。
研究背景:在肺动脉高压 (PAH) 中,没有比较初始三联口服治疗与初始双口服治疗的数据。
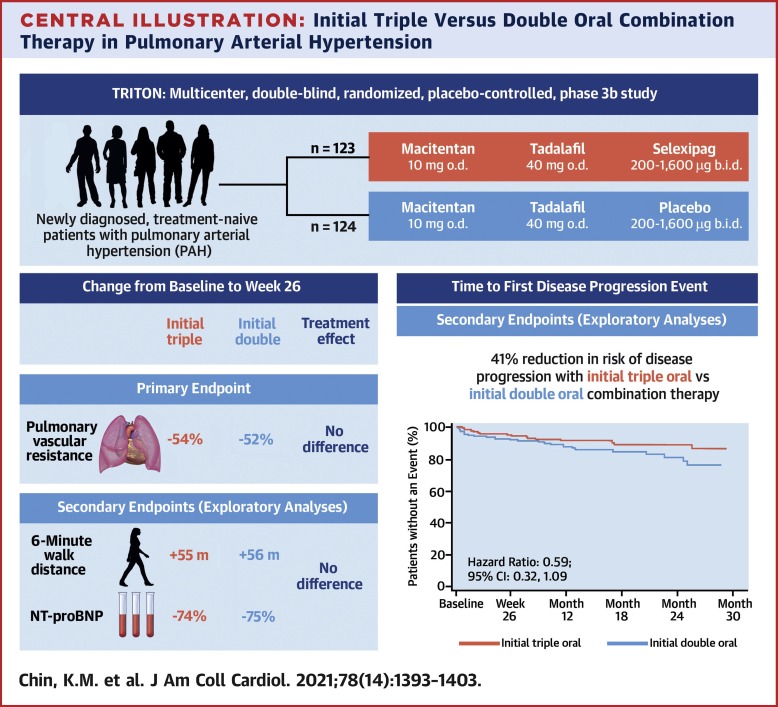
研究目标:TRITON(新诊断肺动脉高压患者初始三联疗法与初始双重口服联合治疗的疗效和安全性;NCT02558231),一项多中心、双盲、随机 3b 期研究,评估初始三联疗法(马西替坦、他达拉非和selexipag)与初始双重(macitentan、他达拉非和安慰剂)口服治疗在新诊断、未接受过治疗的 PAH 患者中的比较。
研究方法:评估疗效直到最后一名随机完成的患者第 26 周(主要观察期结束)。主要终点是第 26 周肺血管阻力 (PVR) 的变化。
研究结果:患者被分配到初始三联疗法(n = 123)或初始双重疗法(n = 124)。在第 26 周,与基线相比,两种治疗策略都降低了 PVR(分别降低了 54% 和 52%),组间没有显着差异。 6 分钟步行距离和 N 端脑钠肽前体在第 26 周有所改善,组间无差异。初始三联疗法与初始双重疗法相比,疾病进展(至主要观察期结束)的风险降低。初始三联疗法最常见的不良事件包括头痛、腹泻和恶心。到主要观察期结束时,初始三联治疗组 2 例患者和初始双联治疗组 9 例患者死亡。
研究结论:在新诊断的 PAH 患者中,两种治疗策略在第 26 周时显着降低了 PVR,两组之间没有显着差异(未达到主要终点)。探索性分析表明,初始三联口服治疗与初始双口服治疗相比,可能是改善长期结果的信号。
文章出处:Chin KM. Three- Versus Two-Drug Therapy for Patients With Newly Diagnosed Pulmonary Arterial Hypertension. J Am Coll Cardiol. 2021 Oct 5;78(14):1393-1403. DOI: 10.1016/j.jacc.2021.07.057. PMID: 34593120.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#肺动脉高压患者#
40
#长期预后#
0
#动脉高压#
0
#JACC#
30
#ACC#
30
不错,学习了
48