Lancet:奥帕他汀可有效治疗中重度特异性皮炎成年和青少年患者!
2021-05-21 MedSci原创 MedSci原创
奥帕他汀作为联合疗法在中重度特异性皮炎的成年和青少年患者中具有积极的获益
特应性皮炎是一种常见的慢性复发性炎性皮肤病,表现为皮肤干燥、湿疹样皮疹和剧烈瘙痒。中重度特应性皮炎一般采用全身疗法与局部皮质类固醇激素联合治疗,可逐渐缓解或暂时痊愈,但可复发。
奥帕他汀(Upadacitinib)是一种口服的Janus激酶(JAK)抑制剂,对JAK1的抑制作用比正在接受异位性皮炎测试的JAK2、JAK3或酪氨酸激酶2更强。
本研究是一项随机、双盲、安慰剂为对照的3期临床试验(AD Up),旨在评估奥帕他汀联合局部皮质类固醇与安慰剂相比在中重度特应性皮炎治疗中的疗效和安全性。
从22个国家的171个临床中心招募了中重度的慢性特应性皮炎成年患者(18-75岁)和青少年患者(12-17岁)(受影响的体表面积≥10%;湿疹面积和严重程度指数[EASI]评分≥16;vIGA-AD评分≥3;每周平均最差瘙痒症数字评分量表分数≥4)。受试患者被随机分至三组(1:1:1),分别接受奥帕他汀 15mg、奥帕他汀 30mg或安慰剂(1/日),联合外用皮质类固醇治疗16周。主要终点是16周时EASI评分较基线降低至少75%的患者比例(EASI-75)和获得vIGA-AD反应的患者比例(vIGA-AD评分 0或1分)。
2018年8月9日-2019年12月20日,共有901位患者被随机分至三组:奥帕他汀 15mg组 300人、奥帕他汀 30mg组 297人、安慰剂组 304人。
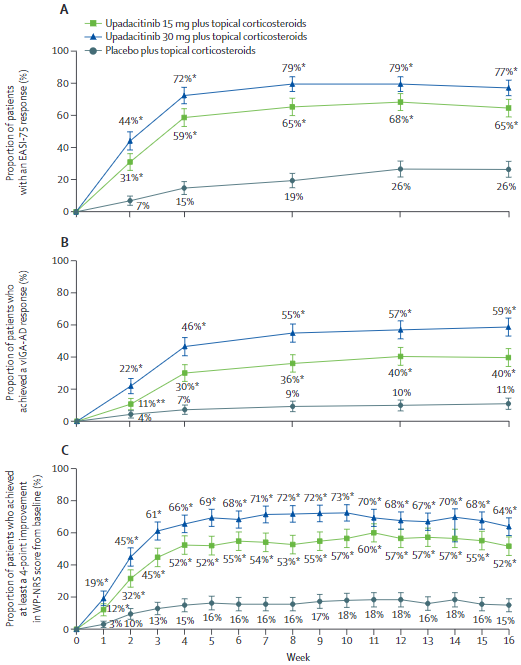
三个治疗组各项主要评估指标的变化
第16周时,奥帕他汀 15mg或30mg联合外用皮质类固醇治疗的患者获得EASI-75的比例明显高于安慰剂组(65% vs 77% vs 26%;与安慰剂组相比的EASI-75反应率的校正差分别是38.1%[15mg]和50.6%[30mg];p<0.0001)。16周时,15mg组和30mg组获得vIGA-AD缓解的患者比例也明显高于安慰剂组(40% vs 59% vs 11%;校正差:28.5%和47.6%;p<0.0001)。
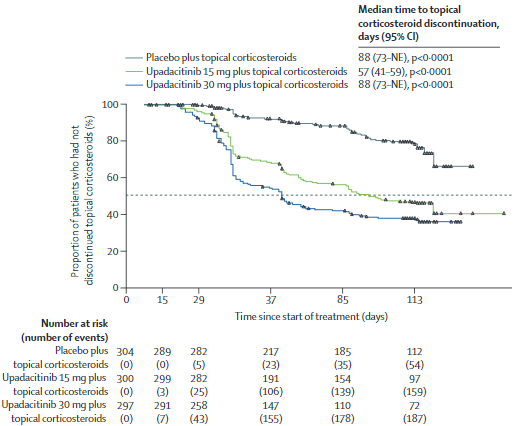
获得EASI-75的患者停用皮质类固醇的时间
在双盲阶段,奥帕他汀 15mg和30mg联合外用皮质类固醇的耐受性均较好。最常见的需紧急治疗的不良反应有痤疮、鼻咽炎、上呼吸道感染、口腔疱疹、血肌酸磷酸激酶水平升高、头痛和特应性皮炎。痤疮在15mg和30mg组的发生率明显高于安慰剂组(10% vs 14% vs 2%)。各组间的导致研究药物中断的不良反应和重度不良反应的发生率相近。无治疗相关死亡。
奥帕他汀联合局部糖皮质激素耐受性良好,疗效明显优于安慰剂联合局部糖皮质激素。奥帕他汀作为联合疗法在中重度特异性皮炎的成年和青少年患者中具有积极的获益-风险特征。
原始出处:
Kristian Reich, et al. Safety and efficacy of upadacitinib in combination with topical corticosteroids in adolescents and adults with moderate-to-severe atopic dermatitis (AD Up): results from a randomised, double-blind, placebo-controlled, phase 3 trial. The Lancet. May 20, 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










非常感谢
31
#Lancet#
36
#特异性#
30
#有效治疗#
31
顶刊就是不一样,质量很高,内容精彩!学到很多
50
好文章!
61