【病史临床】
女性,鼻塞1年余,左侧进行性鼻、面部肿胀2月,反复发热10日。
【影像图片】
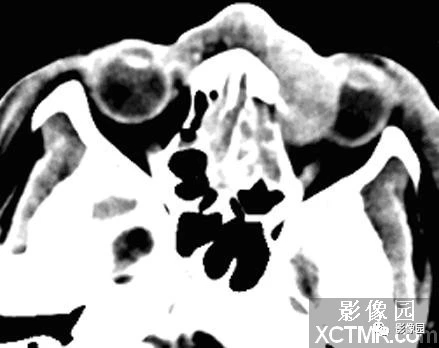
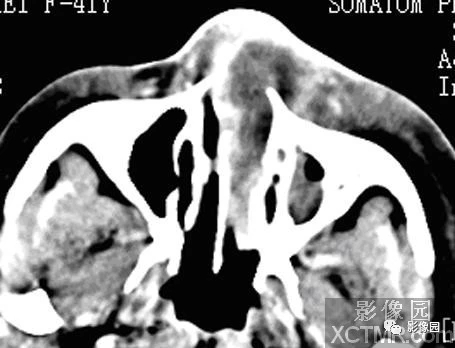

以上三幅图分别为CT增强动脉期、动脉期及延迟期
【影像表现】
横断扫描示左侧鼻腔内可见软组织密度影,增强扫描呈中度强化,病变累及双侧鼻翼、左侧鼻腔及左侧眼眶。双侧鼻翼可见明显肿胀,左侧眼球可见明显受压变扁。骨质明显破坏不明显。
【诊断】
【鉴别诊断】
1.鼻腔内翻状乳头状瘤 2.鼻腔癌 3.鼻息肉
【讨论】
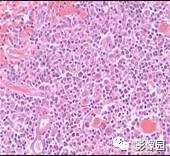
鼻腔鼻窦淋巴瘤在亚洲发病率高,占全部淋巴瘤的2.6%~6.7%,约占结外淋巴瘤的44%,鼻腔鼻窦淋巴瘤大多数为非霍奇金淋巴瘤,根据免疫组织化学分为B、T和T/NK细胞3种类型。B型淋巴瘤最少见,T/NK型最常见,多发生于鼻腔。T细胞型淋巴瘤也常发生于鼻腔,单独发生在鼻窦罕见,预后较T/NK细胞型好。
临床表现包括鼻塞、面颊或鼻区肿胀,还可有流涕、涕血、发热、复视、视物模糊、头痛、眼球突出、颅神经麻痹等。鼻内镜检查显示鼻黏膜坏死、溃疡出血、表面常有恶臭的干痂或脓痂。晚期T/NK细胞型患者常发生鼻骨、鼻甲、鼻中隔或硬腭广泛骨质破坏。甚至面部严重变形。
CT诊断要点:1.病变多发生鼻腔前部;2.病灶密度不均匀,内常有坏死低密度组织;3.骨质常未见明显的破坏;4.病变范围较大时常累及双侧鼻翼及肿瘤周围软组织;5.增强扫描呈较均匀中度强化。
与鼻息肉的鉴别:常发生在中鼻道、下鼻甲后端,病灶密度常不均匀,增强扫描周边黏膜呈波浪状或锯齿状强化,而内容物不强化。
与鼻腔癌的鉴别:典型表现为不规则软组织肿块伴明显骨质破坏,密度不均匀,颈部淋巴结转移少见。
与内翻状乳头状瘤的鉴别:起源于中鼻甲附近的鼻腔外侧壁,易向上颌窦和筛窦蔓延,可侵犯临近的骨质,向鼻腔前部及鼻前庭生长少见,一般不浸润鼻翼及邻近的皮肤。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#细胞性#
33
学习了,谢谢作者分享!
82
学习了,谢谢作者分享!
86
#CT病例#
42
#淋巴结#
31
#鼻腔#
40
不错的.学习了.谢谢分享!
66