GIE: 射频消融可明显降低巴雷特食管低度不典型增生的进一步发展
2020-10-04 MedSci原创 MedSci原创
巴雷特食管炎(BE)是食管腺癌的癌前病变,这种疾病的发病率不断上升。
巴雷特食管炎(BE)是食管腺癌的癌前病变,这种疾病的发病率不断上升,患者会逐步从非增生性肠上皮化生(IM)发展至低度不典型增生(LGD),高度不典型增生(HGD)以及最终浸润性癌症。当前的国际指南建议内镜治疗伴有HGD或早期的BE需行内镜切除术(ER)或射频消融术(RFA)。本项研究的目的是探究射频消融术(RFA)对于降低巴雷特食管炎

研究人员将确诊LGD的BE患者随机分配至RFA或监测保守治疗组。主要观察结局是BE患者进展为高度不典型增生(HGD)/癌症的速度。纳入本项研究中随机分配至RFA(n = 68)或监测(n = 68)组的共有136例患者。研究结束后,根据患者的喜好和研究结果,对15名监测患者进行了RFA癌变的风险的分析。

研究结果显示:从随机分组到最后一次内镜检查的中位随访时间为73个月。在RFA组中有1名患者(1.5%)最后被诊断出HGD /癌症,在监测组中有23名(33.8%)被诊断出HGD /癌症( P = .0001),因此绝对风险降低了32.4%(95%置信区间[CI] ],22.4%-44.2%)。用RFA治疗BE的83例患者中有75例(90%; 95%CI,82.1%-95.0%)达到了BE的完全清除和不典型增生。75例患者中有7例(9%; 95%CI,4.6%-18.0%)复发。
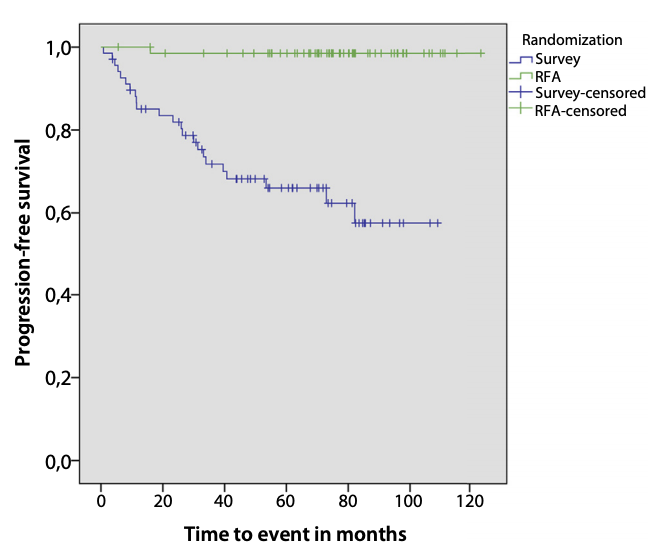
经本项研究证实,患有LGD的BE患者行RFA后显着降低了恶性进展的风险。
原始出处:
Roos E. Pouw. Et al. Radiofrequency ablation for low-grade dysplasia in Barrett’s esophagus: long-term outcome of a randomized trial. Gastrointestinal Endoscopy.2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习了
51
#不典型#
0
#不典型增生#
46
#射频消融#
36
#巴雷特食管#
29
#消融#
26
#食管#
30