Brit J Cancer:男性乳腺癌患者采用他莫昔芬治疗的生存获益
2020-05-05 MedSci原创 MedSci原创
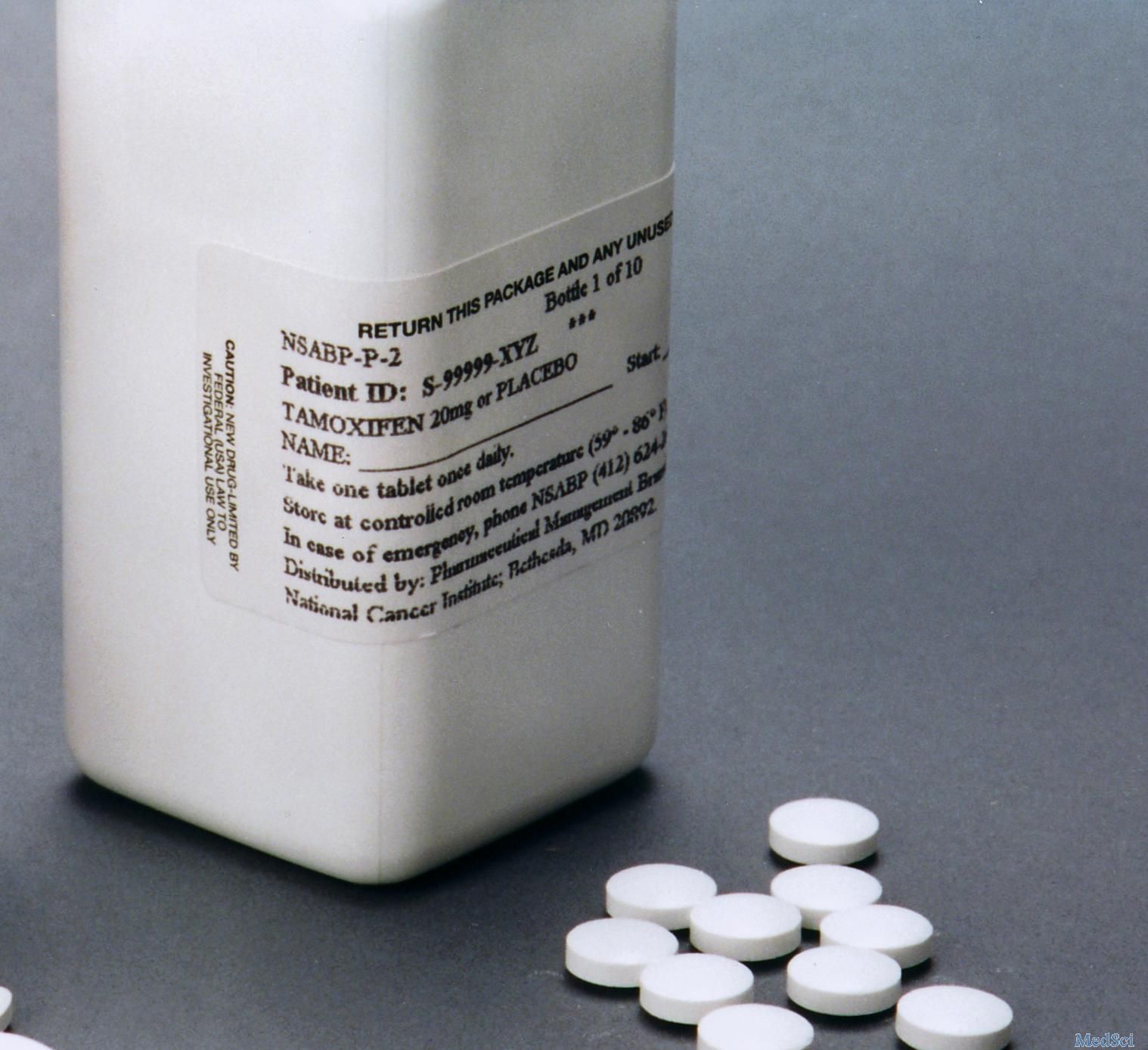
他莫昔芬治疗与MBC患者的DFS改善有关。
由于缺乏前瞻性数据,目前男性乳腺癌(MBC)的治疗主要是基于回顾性分析或女性患者研究得出的信息。近日,肿瘤领域权威杂志British Journal of Cancer上发表了一篇研究文章,在这项前瞻性的队列研究中,研究人员回顾性地分析他莫昔芬在MBC患者中的生存疗效。
在这项前瞻性的队列研究中,从2009年5月至2018年6月期间,研究人员对448例MBC患者进行了治疗,该研究的主要终点是无病生存期(DFS)。
在2009年5月至2018年6月之间,研究人员共确定了448名乳腺癌患者,受试者诊断时的中位年龄为69岁(27-96岁)。中位随访时间为39个月(范围为3-89个月)。多数肿瘤大于20mm。浸润性导管癌没有特殊的组织学类型,分化程度中等。几乎一半的男性患者被诊断出腋窝淋巴结阳性(43.5%)。在98.4%的患者中观察到激素受体(HR)阳性。值得注意的是,与接受他莫昔芬治疗的男性相比,未接受他莫昔芬治疗的男性DFS显著降低(P=0.002)。接受他莫昔芬治疗的患者的复发率和死亡率分别为18.2%和11.2%。最常见的转移部位是骨骼。调整预后因素后,研究人员发现他莫昔芬可将复发率降低68%(风险比HR=0.32;95%置信区间为0.14-0.74)。
由此可见,他莫昔芬治疗与MBC患者的DFS改善有关。
原始出处:
Holm Eggemann,et al.Survival benefit of tamoxifen in male breast cancer: prospective cohort analysis.British Journal of Cancer.2020.https://www.nature.com/articles/s41416-020-0860-4
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#生存获益#
42
#他莫昔芬#
35
#乳腺癌患者#
36
#男性乳腺癌#
39