Lancet:补充孕酮可降低高风险单胎孕妇34周前早产风险
2021-03-26 MedSci原创 MedSci原创
对于有自然早产史或宫颈短的早产高风险孕妇,孕酮补充可降低单胎高风险人群34周前早产风险,但对于多胎妊娠,其效果不显著
早产是全球最常见的新生儿疾病和死亡率因素之一,欧洲的孕妇早产率为5%,而非洲高达18%。早产儿即使存活,其长期健康风险仍较高,如脑瘫、癫痫、认知残疾、失明或听力丧失。内源性孕酮在维持妊娠十分重要,有研究称,孕酮水平下降是分娩启动的重要因素。

近日研究人员考察了在早产高风险人群中,补充孕酮对早产和新生儿不良结局影响。
本次研究为系统综述及荟萃分析,研究人员收集了截至2019年7月,MEDLINE、Embase、CINAHL、妇幼保健数据库及相关试验资料,涉及无症状早产高风险孕妇接受阴道孕酮、肌注17-羟基孕酮己酸(17-OHPC)或口服孕酮预防早产的临床研究。研究的主要终点为早产和新生儿不良结局。
31项试验纳入本次荟萃分析,包含11644名产妇及16185名子女数据。早产高风险孕妇为有自然早产史或宫颈短女性。研究发现,对于单胎高风险孕妇,阴道孕酮(9项试验,3769名孕妇;相对危险度[RR]0.78)、17-OHPC(5项试验,3053名孕妇;0.83)和口服孕酮(2项试验,181名妇女;0.60)可降低34周前早产风险。补充孕酮对其他出生和新生儿结局有利,但产妇并发症可能增加。涉及双胞胎研究发现,阴道孕酮给药不能减少34周前的早产风险(8个试验,2046名孕妇,RR =1.01),对于双胞胎或三胞胎,17-OHPC也不能减少早产风险(8个试验,2253名孕妇,1.04)。在多胎妊娠中,17-OHPC暴露增加了胎膜早破风险(<34周破裂RR=1.59)。
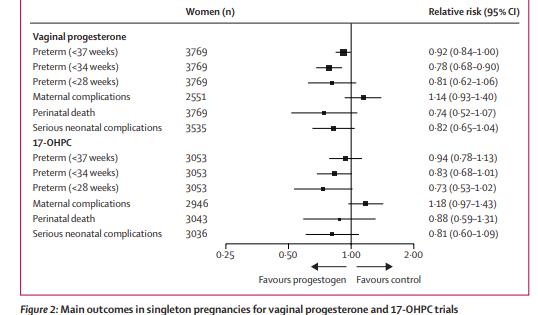
阴道及肌注孕酮对早产风险的影响
研究认为,对于有自然早产史或宫颈短的早产高风险孕妇,孕酮补充可降低单胎高风险人群34周前早产风险,但对于多胎妊娠,其效果不显著。
原始出处:
The EPPPIC Group. Evaluating Progestogens for Preventing Preterm birth International Collaborative (EPPPIC): meta-analysis of individual participant data from randomised controlled trials.Lancet. March 27, 2021.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













学习
42
#Lancet#
31
#高风险#
33
#孕酮#
34
英国妇产杂志上一篇文献报道,对于双胎妊娠,孕11周开始阴道使用孕激素600mg不能降低34周前的早产率,昨天刚看到的😀
95
有用
1
学到了很多东西谢谢老师
0
顶刊就是不一样,质量很高,内容精彩!学到很多
44