J Cell Mol Med:极化巨噬细胞产生的条件培养基对骨髓间充质干细胞细胞行为的影响
2017-12-02 MedSci MedSci原创
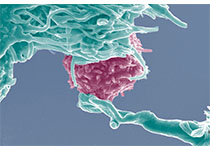
巨噬细胞(Mφs)参与了多种生理和病理过程,包括伤口愈合和组织再生,根据其极化状态,起到正面和负面的作用。在本研究中,我们研究了在由非极化Mφs(M0)或极化Mφs(M1和M2)产生的不同条件培养基(CM)中孵育后骨髓间充质干细胞(BMMSC)的细胞行为。通过使用各种细胞因子刺激诱导Mφ极化,并且在体外基于每个Mφ表型从CM0,CM1和CM2的Mφ培养物获得CMs。结果发现,CM1支持BMMSCs
巨噬细胞(Mφs)参与了多种生理和病理过程,包括伤口愈合和组织再生,根据其极化状态,起到正面和负面的作用。在本研究中,我们研究了在由非极化Mφs(M0)或极化Mφs(M1和M2)产生的不同条件培养基(CM)中孵育后骨髓间充质干细胞(BMMSC)的细胞行为。
通过使用各种细胞因子刺激诱导Mφ极化,并且在体外基于每个Mφ表型从CM0,CM1和CM2的Mφ培养物获得CMs。结果发现,CM1支持BMMSCs的增殖和成脂分化,而CM0对细胞成骨分化有明显影响。CM2在一定程度上也促进了BMMSC的成骨,具体而言,与CM2一起孵育的细胞展现出增强的形成稳健的干细胞片层的能力。尽管与CM1孵育也增加了细胞外基质组分,如纤连蛋白、COL-1和整联蛋白β1,在片材诱导期间的产生,但由CM2孵育的细胞产生的片层比由CM1孵育的细胞产生的片层厚(P <0.001)。
综上所述,该研究结果表明,每个Mφ表型对BMMSC具有独特的作用。移植后微调的Mφ极化可能是调节BMMSCs治疗潜力的有效方法。
原始出处:
He XT, Li X, et al., The effects of conditioned media generated by polarized macrophages on the cellular behaviours of bone marrow mesenchymal stem cells. J Cell Mol Med. 2017 Nov 6. doi: 10.1111/jcmm.13431.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#骨髓间充质干细胞#
41
#间充质干细#
23
#Cell#
39
#CEL#
24
#Med#
25