NEJM:支气管瘘引起的颅腔积气-病例报道
2020-05-21 MedSci原创 MedSci原创
颅腔积气被认为是源自支气管瘘的空气栓塞所致。该患者后来在重症监护室内死亡。
患者为一名患有肺IIIB期鳞状细胞癌的61岁男子,在医院接受再分期计算机断层扫描(CT)时出现癫痫样活动。
他的肺脏右下叶有一个明确的原发性空洞病变,曾接受过三个周期的卡铂和纳米粒子结合白蛋白的紫杉醇(Abraxane)治疗。他被转移至急诊室,突然出现呼吸衰竭和神志不清,进行了紧急插管。
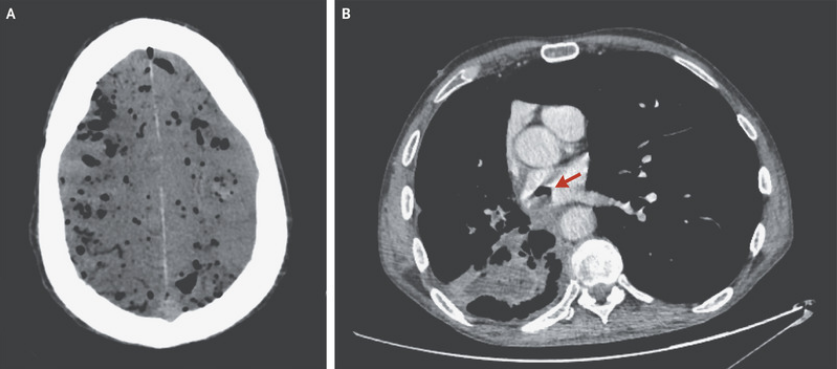
头颅CT显示弥漫性颅腔积气(如图A所示)。对胸部进行的分期CT扫描显示右下叶既往明确的空洞病变在支气管和左心房之间形成了瘘管(如图B箭头所示)。
颅腔积气被认为是源自支气管瘘的空气栓塞所致。该患者后来在重症监护室内死亡。
原始出处:
Alan Zakko,et al.Pneumocephalus Due to a Bronchoatrial Fistula.N Engl J Med 2020;https://www.nejm.org/doi/full/10.1056/NEJMicm1912126
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#支气管#
31
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
40
了解一下
83