Circulation:过敏毒素受体C3aR参与调节血小板功能和动脉血栓形成原始出处:
2018-10-23 MedSci MedSci原创
血小板在血管系统中具有独特的功能,既是血栓形成的主要介质,对恢复组织完整性至关重要,又在血管炎症环境下发挥重要作用。补体系统是抵御微生物入侵的第一道防线,是炎症的重要介质。虽然补体和凝血系统之间的液相交叉很受重视,但其相互作用的病理生理意义尚不明确。研究人员采用流式细胞术分析了501位冠状动脉疾病患者血小板上激活的糖蛋白IIb/IIIa和过敏毒素受体C3aR共表达的情况;采用qPCR、免疫荧光、W
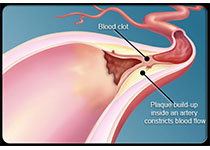
血小板在血管系统中具有独特的功能,既是血栓形成的主要介质,对恢复组织完整性至关重要,又在血管炎症环境下发挥重要作用。补体系统是抵御微生物入侵的第一道防线,是炎症的重要介质。虽然补体和凝血系统之间的液相交叉很受重视,但其相互作用的病理生理意义尚不明确。
研究人员采用流式细胞术分析了501位冠状动脉疾病患者血小板上激活的糖蛋白IIb/IIIa和过敏毒素受体C3aR共表达的情况;采用qPCR、免疫荧光、Western blotting或流式细胞术检测人或小鼠C3aR的表达水平;同时采用多种体外血小板功能试验、活体出血时间和活体镜检法检验血小板C3aR的重要性。通过心肌梗死和中风的疾病模型来观察C3aR的病理生理相关性。此外,研究人员还采用纳米级液相色谱与串联质谱联合鉴定血小板小GTPase Rap1b,来探究潜在的分子机制。
研究人员发现在冠状动脉疾病患者中,血小板补体C3aR的表达和激活的糖蛋白IIb/IIIa呈正相关,而且C3aR和糖蛋白IIb/IIIa在心肌梗死患者的血栓中共表达。研究人员还发现血小板上的C3a/C3aR轴可调节血栓形成的不同步骤,例如血小板黏附、扩张和Ca2+内流。通过给C3aR-/-或C3-/-小鼠注射C3a,研究人员发现补体激活片段C3a可调节尾巴受伤和血栓后的出血时间。值得注意的是,C3aR-/-小鼠不容易发生实验中风和心肌梗死。而且,用C3aR+/+血小板调整C3aR-/-小鼠和敲除血小板的实验表明研究过程中所观察到的对血栓形成、心肌梗死和中风的效应是由血小板C3aR引起的。机制上,即在受伤或者体内血栓形成后,C3aR介导的信号调节激活Rap1b,进而阻断出血。
总体上,本研究揭示了过敏毒素C3a在血小板功能和血栓形成方面的新功能,强调了心血管疾病中补体激活失衡的有害作用。
原始出处:
Reinhard J. Sauter,et al.Functional Relevance of the Anaphylatoxin Receptor C3aR for Platelet Function and Arterial Thrombus Formation Marks an Intersection Point Between Innate Immunity and Thrombosis. Circulation.July 24,2018;138:1720–1735
本文系梅斯医学(MedSci)原创编译,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#动脉血#
31
#C3aR#
30
#原始出处#
42
#动脉血栓#
46
#动脉血栓形成#
34
#动脉血栓形成#
37
了解一下,谢谢分享!
70