颈内动脉支架成形术后高灌注综合征3例分析
2019-04-27 李颜 白小欣 蔡军 中西医结合心脑血管病杂志
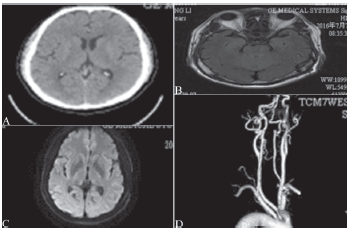
病例[1],男,55岁,2012年7月因“右手指麻木半月余”入院。查体未见明显阳性体征,诊断为脑梗死、高血压,血压控制情况不详。TCD提示右侧大脑中动脉低流速、低搏动改变。入院DSA提示右侧颈内动脉起始段重度狭窄(85%),左侧椎动脉开口重度狭窄。入院第6天在局部麻醉下于右侧颈内动脉起始段、左侧椎动脉开口行支架成形术,术中使用保护伞,术后第1天诉少许头痛,其间血压波动在(140~147)/(80~
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#成形术#
24
#高灌注综合征#
27
#高灌注#
39
#综合征#
24
#颈内动脉#
35