CORR:创伤性肘关节不稳影像学诊断的可信度良好
2013-05-29 CORR dxy
肘关节部位骨折合并关节脱位发生率较低,因而创伤外科医生对该疾病诊断可能并没有像其他部位骨折一样来的准确。对肘关节骨折类型的判断可以较为精确地评估患者软组织损伤程度和骨折的发生机制,为后续治疗提供参考。目前尚无创伤骨科医生评估肘关节骨折分型精确性和一致性的研究报道,近日来自美国的学者就此进行了相关研究,并阐述了下列问题:1.骨科医生对创伤性肘关节不稳定骨折分型的组间一致性;2.影像学诊断肘关节骨折类
肘关节部位骨折合并关节脱位发生率较低,因而创伤外科医生对该疾病诊断可能并没有像其他部位骨折一样来的准确。对肘关节骨折类型的判断可以较为精确地评估患者软组织损伤程度和骨折的发生机制,为后续治疗提供参考。目前尚无创伤骨科医生评估肘关节骨折分型精确性和一致性的研究报道,近日来自美国的学者就此进行了相关研究,并阐述了下列问题:1.骨科医生对创伤性肘关节不稳定骨折分型的组间一致性;2.影像学诊断肘关节骨折类型的准确性。
研究者在网络上发出调查邀请,共76位骨科医生接受邀请,73位(96%)医生完成调查。调查问卷的组成为53例肘关节骨折患者的影像学X片,入选X片符合以下标准:创伤性肘关节不稳定;X片图片清晰;年龄大于18岁。53例肘关节骨折片共有:桡骨头骨折伴后脱位(7例);恐怖三联征(19例);内翻后内侧旋转损伤(4例);尺骨鹰嘴骨折伴肘关节前脱位(5例);尺骨鹰嘴骨折伴肘关节后脱位(18例),如图1所示。所有诊断均经过开放手术确认。
研究结果提示:
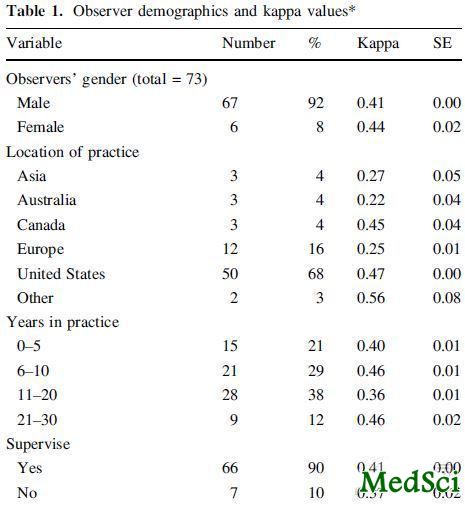
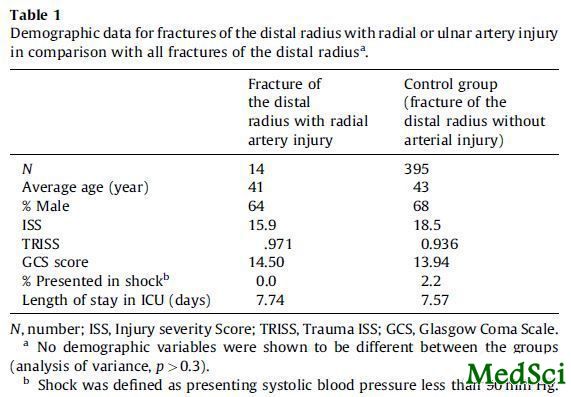
不同骨科医生间的总体组间一致性K=0.41,当对观察者按不同标准进行分组比较后发现,其组间一致性相当,组间一致性和每年治疗的病例数有关,而和手术医生的工作年限无关,即每年治疗肘关节骨折病例数大于5例的医生具有较高的组间一致性,(如表1所示)。

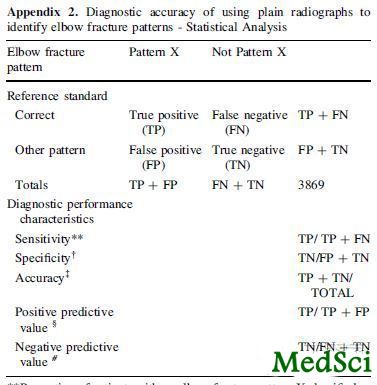
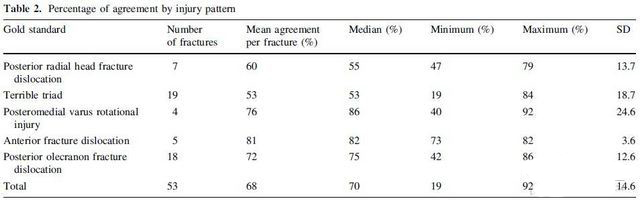
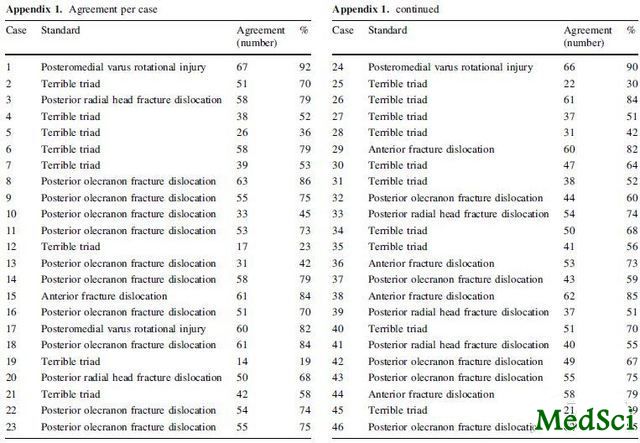
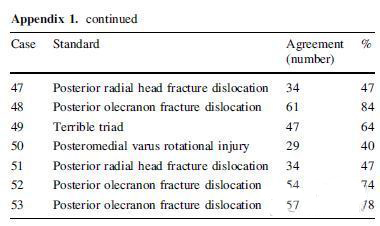
观察者的总体诊断诊断准确率在80%,范围在76%-93%之间浮动,其中诊断尺骨鹰嘴骨折的准确率最好,诊断肘关节恐怖三联征准确率最低(如表2,3,附录1,2所示)。
表2:损伤类型的一致性百分比
表3:影像学诊断准确性的分布
附录2:肘关节骨折诊断准确性的分布
研究者认为:创伤性肘关节不稳定诊断在不同骨科医生间中等程度的一致性,并且其精确性尚可接受。

Diagnosis of elbow fracture patterns on radiographs: interobserver reliability and diagnostic accuracy.
BACKGROUND
Studies of traumatic elbow instability suggest that recognition of a pattern in the combination and character of the fractures and joint displacements helps predict soft tissue injury and guide the treatment of traumatic elbow instability, but there is no evidence that patterns can be identified reliably.
QUESTIONS/PURPOSES
We therefore determined (1) the interobserver reliability of identifying specific patterns of traumatic elbow instability on radiographs for subgroups of orthopaedic surgeons; and (2) the diagnostic accuracy of radiographic diagnosis.
METHODS
Seventy-three orthopaedic surgeons evaluated 53 sets of radiographs and diagnosed one of five common patterns of traumatic elbow instability by using a web-based survey. The interobserver reliability was analyzed using Cohen's multirater kappa. Intraoperative diagnosis was the reference for fracture pattern in calculations of the sensitivity, specificity, accuracy, and positive predictive and negative predictive values of radiographic diagnosis.
RESULTS
The overall interobserver reliability for patterns of traumatic elbow instability on radiographs was κ=0.41. Treatment of greater than five such injuries a year was associated with greater interobserver agreement, but years in practice were not. Diagnostic accuracy ranged from 76% to 93% and was lowest for the terrible triad pattern of injury.
CONCLUSIONS
Specific patterns of traumatic elbow instability can be diagnosed with moderate interobserver reliability and reasonable accuracy on radiographs.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#影像学诊断#
65
#创伤性#
56
#肘关节#
51
#创伤#
56
#ORR#
46