盘点:黑色素瘤近期重要研究进展一览
2018-06-30 MedSci MedSci原创
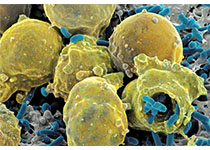
黑色素瘤,又称恶性黑色素瘤,是来源于黑色素细胞的一类恶性肿瘤,常见于皮肤,亦见于黏膜、眼脉络膜等部位。黑色素瘤是皮肤肿瘤中恶性程度最高的瘤种,容易出现远处转移。早期诊断和治疗因而显得尤为重要。这里梅斯小编整理了近期关于黑色素瘤的重要研究进展,与大家一同分享。【1】Pembrolizumab联合聚乙二醇干扰素或Ipilimumab治疗晚期黑色素瘤或肾细胞癌Pembrolizumab单药,Ipil
黑色素瘤,又称恶性黑色素瘤,是来源于黑色素细胞的一类恶性肿瘤,常见于皮肤,亦见于黏膜、眼脉络膜等部位。黑色素瘤是皮肤肿瘤中恶性程度最高的瘤种,容易出现远处转移。早期诊断和治疗因而显得尤为重要。这里梅斯小编整理了近期关于黑色素瘤的重要研究进展,与大家一同分享。
【1】Pembrolizumab联合聚乙二醇干扰素或Ipilimumab治疗晚期黑色素瘤或肾细胞癌
Pembrolizumab单药,Ipilimumab单药或聚乙二醇干扰素(PEG-IFN)单药对黑色素瘤和肾细胞癌均有抗肿瘤活性。KEYNOTE-029临床研究探究了Pembrolizumab联合Ipilimumab或PEG-IFN对晚期黑色素瘤或肾细胞癌的抗肿瘤活性。研究包括独立的Pembrolizumab联合低剂量Ipilimumab和Pembrolizumab联合PEG-IFN队列。18例患者中少于等与6例患者出现剂量限制毒性(DLT)则认为Pembrolizumab 2mg/kg每3周(Q3W)联合4次剂量的Ipilimumab 1mg/kgQ3W耐受性良好。Pembrolizumab2mg/kg Q3W联合PEG-IFN的目标DLT率为30%。Ipilimumab队列纳入22例患者,19例患者可进行DLT评估。6例患者出现≥1DLT。13例患者出现3-4级治疗相关不良反应。12例黑色素瘤患者中5例出现治疗反应,10例肾细胞癌患者中3例出现治疗反应。PEG-IFN队列中,接受剂量水平1治疗的14例患者中2例出现DLT,接受剂量水平2治疗的3例患者2例出现DLT。17例患者中有10例患者出现治疗相关不良反应。5例黑色素瘤患者1例出现治疗反应,12例肾细胞癌患者2例出现治疗反应。
【2】黑色素瘤患者血浆中循环肿瘤DNA的液体分析用于伴随诊断和BRAF抑制剂治疗的监测
目前对于确定BRAF靶向治疗转移性黑色素瘤患者资格的标准是基于组织的BRAF突变检测。由于患者很少进行再次手术,通过实时全面评估肿瘤突变状态,从而在血液中检测可能是有利的,这也代表监测BRAF治疗的无创生物标志物。研究总共有634例I〜IV期黑素瘤患者被纳入到2个中心,并前瞻性收集1406例血浆标本。结果发现,血浆和组织检测结果之间高度一致。值得注意的是,在某些情况下,与BRAFi无应答或继发性BRAF突变恶性肿瘤相关的结果存在差异。重要的是,ctDNA结果与95.7%的疾病临床过程和治疗反应相关。值得注意的是,BRAF突变ctDNA 的检测先于实体瘤反应评估标准评估的复发,并且比血清S100和乳酸脱氢酶更具特异性。表明基于血液的检测与基于标准组织的BRAF突变检测相当。重要的是,即使对于早期患者,基于血液的BRAF检测也与临床病程相关,并且可用于预测BRAFi治疗下放射成像前对治疗,复发和耐药的反应,从而显著改善患者治疗。
【3】MAGE-A3免疫疗法用于黑色素瘤无治疗效果
尽管有新批准的治疗方法,转移性黑色素瘤仍是一种危及生命的疾病。研究人员对MAGE-A3免疫疗法治疗IIIB或IIIC期黑色素瘤患者的效果进行评估。研究人员在31个国家的263个中心开展一双盲的、随机的、安慰剂对照的III期临床试验,招募年满18岁的组织学确诊的、完全确诊的、MAGE-A3阳性的IIIB或IIIC期皮肤黑色素瘤患者,并要求有肉眼可见的淋巴结侵及、ECOG表现评分0或1分。将患者按2:1随机分至实验组(300ug MAGE-A3抗原+420ug CpG7909,溶于AS01B,总0.5mL,肌肉注射)或安慰剂组;前5次用药间隔3周、后8次用药间隔12周,共13次,持续27个月。共筛选到1345位患者参与试验。结果显示,在GS阳性人群中,实验组和对照组的中位无病存活期分别是9.9个月和11.6个月。在治疗前31天,实验组894位患者中有126位(14%)、对照组450位患者中有56位(12%)患者出现3级及以上副反应;治疗相关的3级及以上副反应分别是36例(4%)vs 6例(1%);此外,两组均有14%的患者至少出现一次严重副反应事件。在这种临床环境下单用抗原特异性的免疫疗法是无效的。基于本研究结果,停止探究MAGE-A3免疫疗法用于治疗黑色素瘤。
【4】最初诊断的黑色素瘤能够增加随后患前列腺癌风险
越来越多的证据表明,皮肤黑色素瘤的诊断(CM)也许与前列腺癌的发生率(PC)相关。最近,有研究人员调查了是否CM的发生率与随后PC风险的增加相关。研究人员利用来自新南威尔士癌症数据库中的所有CM和PC案例数据进行了分析,这些案例都在1972年和2008年之间诊断。研究总共包括了143594名诊断为PC或者CM的男性,其中第一主要癌症的PC患者和CM患者分别包括101198名和42396名。研究发现,PC发生的风险随着CM的诊断增加,并且在诊断为局部CM的患者中风险明显增加。最后,研究人员指出,CM的诊断能够增加随后PC发生的风险。另外,新诊断为CM的男性应该考虑未来PC风险的可能。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#色素#
14
#研究进展#
14
#黑色素#
21
#黑色素#
30
学习学习
32
了解一下.谢谢分享!
38