盘点:JACC三月第一期研究一览
2019-03-11 不详 MedSci原创
1.操作时间对血管内血栓切除术预后的影响研究<span style="mso-spacerun:'yes';font-family:Calibri;mso-fareast-font-family:宋体; mso-bidi-font-family:'Times New Roman';font-size:10.5000pt;mso-font-kerning:1.0000pt;">DOI: 10.10
DOI: 10.1016/j.jacc.2018.11.052
血管内血栓切除术(ET)是目前治疗急性缺血性卒中的标准方法,尽管成功的ET可以明显改善患者预后,但是更长的操作时间(PT)与更低的功能独立率相关。本研究的目的旨在评估操作时间对ET术后患者的预后和并发症的影响。本研究纳入了来自7个美国医疗中心的1359名接受ET治疗的患者,分析结果显示当操作时间超过30min后会降低患者的预后(p < 0.01),术后出血率和并发症发生率随着操作时间呈指数增加。成功再通的累积率和良好的预后在PT超过60min后达到稳定期。在PT>30min的患者中,更少的尝试可以预测ET的成功和良好的预后(p < 0.01)。研究结果显示,在接受血管内血栓切除术治疗的患者中,操作时间越长,术后出血和并发症的发生风险越高。
DOI: 10.1016/j.jacc.2018.11.049
进行性恶化的心衰伴射血分数降低(HFrEF)患者的流行病学特征尚不完整。本研究的目的旨在评估进行性恶化的HFrEF患者的发病率、临床特征、治疗和预后。本研究纳入分析了11064名HFrEF患者,其中1851名(17%)患者在平均1.5年后发展为进行性恶化的HFrEF患者。发展为进行性恶化的HFrEF患者更多的是非洲裔美国人,年龄多在80-90岁之间,并发症的负担更高(p < 0.001)。在进行性恶化HF形成后,42.4%的患者接受的是单一疗法,43.4%的患者接受的是双重疗法,14.1%的患者接受的是三重疗法。总共48%、61%和98%的患者分别接受了血管紧张素转换酶抑制剂/血管紧张素受体阻滞剂、β受体阻滞剂和盐皮质激素受体拮抗剂的目标剂量>50%的治疗。另外,患者2年的死亡率是22.5%,56%的患者在发展为进行性恶化HF的30天内再住院治疗。研究结果显示,有约六分之一的心衰伴射血分数降低的患者会在诊断后18个月内发展为进行性恶化的心衰,这些患者的2年死亡率和再住院风险明显更高。
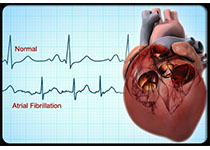
DOI: 10.1016/j.jacc.2018.11.051
目前,对于非瓣膜性房颤(AF)和极低体重(50kg)患者,直接口服抗凝药物(DOACs)的有效性和安全性尚不清楚。本研究的目的旨在评估和比较DOACs和华法林对极低体重AF患者的效果。本研究纳入了韩国国家数据库中的接受口服抗凝药物治疗的体重≤60kg的AF患者(DOACs n=14013;华法林 n=7576),并用倾向性评分调整两组患者。分析结果显示,与华法林相比,DOACs 与更低的缺血性卒中([HR]: 0.591; 95% [CI]: 0.510-0.686)和主要出血事件相关(HR: 0.705; 95%: CI 0.601-0.825),而这些均由颅内出血的减少(HR: 0.554; 95% CI: 0.429-0.713)导致。另外,DOACs 可以提高临床净效益(HR: 0.660; 95% CI: 0.606-0.717),这些结果在体重<50kg的患者中是一致的。研究结果显示,对于极低体重AF患者,直接口服抗凝药物的有效性和安全性优于华法林。
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#JACC#
31
很好的学习机会
80
很好的学习机会
75
#ACC#
32
了解一下,谢谢分享!
71