ATVB:血浆n-3和n-6脂肪酸与颈动脉斑块进展之间的相关性有差异!
2018-01-12 xing.T MedSci原创
由此可见,这些发现支持二十二碳六烯酸作为抗动脉粥样硬化的主要营养素,而没有有效的n-6 FAS证据来反驳其促进动脉粥样硬化的作用。
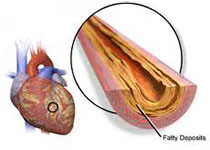
ω-3(n-3)脂肪酸(FAS)一直被认为是一种健康的饮食成分,然而,最近的临床试验已经质疑他们的心血管益处。相比之下,ω-6(n-6)FAS被认为是有害的,致动脉粥样硬化的宏量营养素,尽管缺乏经验证据支持这一假说。近日,心血管领域权威杂志Arteriosclerosis, Thrombosis, and Vascular Biology上发表了一篇研究文章,研究人员旨在通过3327名多民族动脉硬化研究(MESA)研究来明确血浆n-3和n-6FAS是否与颈动脉斑块风险及其进展相关。
在基线和中位期为9.5年后,研究人员进行超声检查评估颈动脉斑块,并采用气相色谱-火焰离子化检测器测定血浆磷脂n-3和n-6 FAS。对典型心血管疾病危险因素进行调整后,通过相对风险回归分析评估了FAS与颈动脉斑块的存在或进展之间的关系。
在基线时,研究人员发现n-3二十二碳六烯酸含量位于第四个四分位数范围的参与者中显示颈动脉斑块的风险降低9%(P=0.05),而在n-3α-亚麻酸位于第二个四分位数范围的参与者中显示颈动脉斑块的风险增加11%,与相应的参照组相比(P=0.02)。在前瞻性分析中,在9.5年期间,二十二碳六烯酸位于最高四分位数的参与者中显示颈动脉斑块进展的风险降低12%,与相应的参考四分位数组别相比(P=0.002)。其中n-6 FAS和斑块的结局并没有观察到显著的关系,也没有发现显著的种族/民族交互作用。
由此可见,这些发现支持二十二碳六烯酸作为抗动脉粥样硬化的主要营养素,而没有有效的n-6 FAS证据来反驳其促进动脉粥样硬化的作用。
原始出处:
Brian T. Steffen,et al. Plasma n-3 and n-6 Fatty Acids Are Differentially Related to Carotid Plaque and Its Progression MESA (the Multi-Ethnic Study of Atherosclerosis).ATVB.2018. https://doi.org/10.1161/ATVBAHA.117.310366
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#TVB#
36
#颈动脉斑块进展#
46
#相关性#
38
学习了.谢谢分享
73
学习了.谢谢分享
100
学习了感谢分享
73
#颈动脉#
37
#颈动脉斑块#
30
#斑块#
33
了解了.谢谢分享!
69