Nature:肿瘤DNA错配修复与免疫治疗响应的相关性
2017-12-07 仗剑书生 “医海拾贝微转化”
应用免疫检测点抑制剂如PD-1与CTLA-4抗体在肿瘤治疗中取得了良好的效果。然而,肿瘤对免疫检测点抑制剂的响应率较低,从而限制了免疫治疗的有效性。对PD-1治疗后非小细胞肺癌进行全外显子测序,发现基因组突变负担(mutation burden)与免疫治疗有效性相关(Science. 2015 348(6230):124-8.)。今年6月份,《Science》再度报道了DNA错配修复的缺失产生的大
应用免疫检测点抑制剂如PD-1与CTLA-4抗体在肿瘤治疗中取得了良好的效果。然而,肿瘤对免疫检测点抑制剂的响应率较低,从而限制了免疫治疗的有效性。对PD-1治疗后非小细胞肺癌进行全外显子测序,发现基因组突变负担(mutation burden)与免疫治疗有效性相关(Science. 2015 348(6230):124-8.)。今年6月份,《Science》再度报道了DNA错配修复的缺失产生的大量新突变(neogantigens)能提高免疫治疗的响应,该研究结论是建立在近3年的免疫治疗临床试验结果的基础上。近期上线的《Nature》详细论述了DNA错配修复与免疫检查点抑制剂响应的相关性。
DNA错配修复是通过修正错配的碱基进行修复,碱基的错配主要来源于DNA复制中的错误。修复的过程主要由相应地蛋白复合物完成,其中包括MLH1、MSH2 、MSH6等。DNA错配修复的缺失导致微卫星不稳定性(microsatellite instability,MSI)。
研究者首先利用cas9技术获得Mlh1敲除的结肠癌细胞,在移植到免疫缺陷小鼠中后,Mlh1敲除组的肿瘤大小与对照相似。然而在移植到免疫正常小鼠中后,Mlh1敲除组的肿瘤大小显着小于对照。
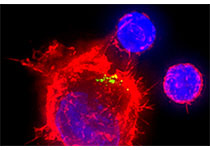
那么内在机理如何呢?DNA错配修复产生了大量的新抗原(neoantigen),是否是新抗原引发了免疫响应呢?研究者接着利用免疫检查点抑制剂PD-1或CTLA-4抗体进行治疗,结果显示DNA错配修复的缺失的肿瘤很好的响应了免疫抑制剂治疗。
本研究揭示了DNA错配修复缺失导致新抗原负担引发了免疫监视,进而提高了免疫检查点抑制剂的响应。由于DNA错配修复相关蛋白与DNA聚合酶具有较好的酶活性(ATP酶与外切酶),因而可作为很好的药物靶点。
原始出处:
Germano G,et al.,Inactivation of DNA repair triggers neoantigen generation and impairs tumour growth.Nature. 2017 Nov 29.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#相关性#
25
#Nat#
34
学习
49