JAMA DERMAT:不可思议!PD-1抗体让癌症患者“白发”变“黑发”
2017-07-15 佚名 生物探索
这几年,PD-1/PD-L1抗体俨然已成为癌症治疗领域的“明星”。近日,科学家们得到了一个关于PD-1/PD-L1抗体的新发现——它们让肺癌患者白发变黑发。这究竟是怎么回事呢?
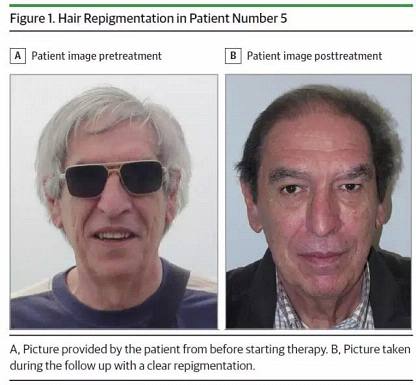 图1(来源:JAMA Dermatology)
图1(来源:JAMA Dermatology)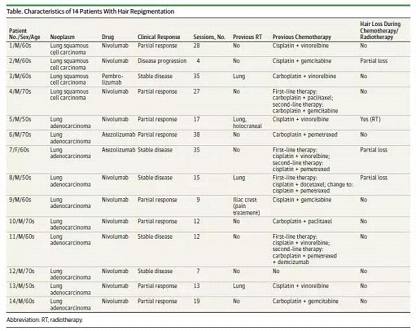

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











还有这种作用?
70
#癌症患者#
30
#PD-1抗体#
35
学习了,谢谢分享
68
感谢小编为我们准备了如此丰盛的精神大餐,同时也向作者致谢!认真学习了,点赞!
53
所以,白发变黑发还是有希望的
59
意想不到收获
64