Eur Heart J:FFR指导下PCI治疗远期预后较优
2013-05-07 Eur Heart J dxy
心血管领域知名杂志European Heart Journal近日在线发表了我国医生撰写的论文"当前医疗实践中,FFR指导与血管造影指导PCI治疗远期预后对比(Long-term outcomes of fractional flow reserve-guided vs. angiography-guided percutaneous coronary intervention in contem
心血管领域知名杂志European Heart Journal近日在线发表了我国医生撰写的论文"当前医疗实践中,FFR指导与血管造影指导PCI治疗远期预后对比(Long-term outcomes of fractional flow reserve-guided vs. angiography-guided percutaneous coronary intervention in contemporary practice)"的研究论文。这是迄今为止,进一步确证以FFR评估指导PCI治疗有效性的研究论文。European Heart Journal隶属于欧洲心脏病学会(European Society of Cardiology),是国际心血管领域的权威期刊,影响因子10.478。本论文发表于该杂志2013年1月23日在线版。
该论文由首都医科大学附属北京宣武医院心内科李静博士等撰写,旨在明确在临床实践中,FFR指导经皮冠脉介入治疗(PCI)的远期预后状况。他们发现对于稳定性冠心病患者,FFR指导的治疗策略远期临床结局较优,认为在进行心脏导管治疗临床决策中应广泛采用FFR评估。
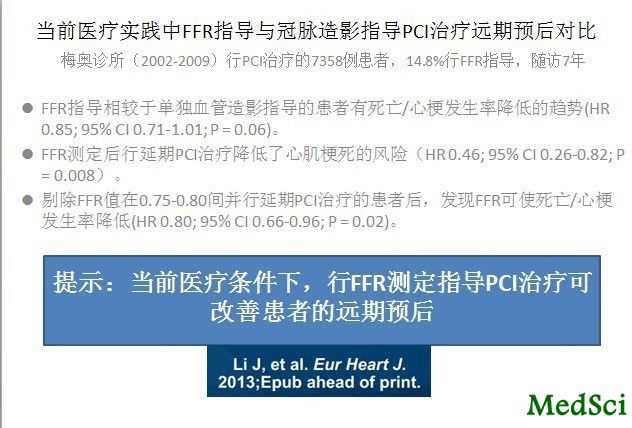
研究采用回顾性队列分析,共纳入了梅奥诊所在2002年10月到2009年12月期间的所有进行PCI术的7358例患者,将其分为两组:有(6268例)或无(1090例)FFR指导下进行PCI。FFR指导组的患者又分两类:行PCI组(FFR后即行PCI,721例),推迟PCI组(FFR评估后延期PCI治疗,369例)。中位随访期为50.9个月,对各组在此期间的临床事件进行对比。
结果显示两组7年时主要心脏不良事件的Kaplan-Meier分数分别为57.0%(无FFR指导组)和50.0%(FFR指导组)(P=0.016)。相较于血管造影指导下的PCI治疗,FFR指导组患者死亡或心梗的发生率较低,但并不显著(HR:0.85,95% CI: 0.71-1.01, P = 0.06);FFR指导的延迟PCI治疗策略与心梗发生率成独立相关关系(HR: 0.46, 95% CI: 0.26-0.82, P = 0.008)。在排除FFR值在0.75-0.80并延期PCI的患者之后,FFR的应用可显著降低死亡和心梗的发生率(HR: 0.80, 95% CI: 0.66-0.96, P = 0.02)。
因此,可作出结论,在目前的医疗实践中,FFR指导的治疗策略远期临床结局较优,应在导管治疗决策中采用FFR指导。
述评:为何不采用正确方法进行临床决策?(Angiography and fractional flow reserve in daily practice: why not (finally) use the right tools for decision-making?"
Li等最近对2002到2009年间梅奥诊所行PCI治疗患者的远期预后数据进行了报道,该数据并不包括因ST段抬高性心肌梗死(STEMI)进行急诊PCI患者。作者着重研究了血流储备分数(FFR)指导临床决策的意义。在排除血管FFR值在0.75-0.80而选择延期PCI治疗的患者后,研究结果充分证明,相对于在临床表现和血管造影的基础上判定行PCI治疗,FFR指导PCI治疗组的死亡和心梗发生率显著降低。这些数据与其他许多报道(随机化或非随机化研究)一致。
Li等也认为单中心观察性、回顾性研究的弱点是该项工作的最大局限。是的,研究未进行随机化可能使得患者的基线状况有所不同。确实,有人可能发现,对不同操作者对于是否应用FFR指导PCI治疗的个人决策所产生的偏倚,即使应用最先进的多元分析以及倾向评分分析也不能解决这一问题。还有人可能对此研究结果不屑一顾,认为诸如此类的注册研究中,FFR应用指南本身可能存在错误,并且指南在研究期间会有所更新。还有人会对临床终点并非预先设定、也无独立的临床事件委员会对事件进行裁定而感到遗憾。还有!FFR的具体情况并未由中心实验室进行检查也是一大硬伤。人们可能还会说……我们在日常临床实践中并不会如此操作。
然而,这些非难忽略了一点,对于用"日常操作"(例如我们每天的所作所为)来治疗患者,细致地报道其远期临床结局是极端重要的。有两个方面值得我们重视:第一,该研究是在临床数据库和本实验室报告系统的基础上做出的。这本身就保证了纳入患者的连续性特点,并对所有患者进行了分析,而不是择优选择之后进行某些随机化控制试验(RCT)。这一连续性特点同很多RCT的缓慢纳入率形成鲜明对比。在COURAGE研究中,平均纳入速率为<1例/月/中心。其余的那些有稳定性冠脉疾病的患者哪里去了?这些数据说明存在"沉默的大多数"--因这样或者那样的原因未能进行随机化,例如偏倚的原因。这样使得RCT结果的临床推广受限,从而使我们认识到注册试验中纳入患者连续性的重要。其次,Li报道中患者随访资料的全面性也可圈可点。在患者接受PCI治疗后,他们分别在6月、12月以及之后每年一次的频率进行电话随访。只有4.2%的患者失随访。若在随机化的对照临床试验中进行类似时长的随访,则失随访率可能是Li研究的2倍。对于PCI患者的远期预后进行精确评估的意义,一点也不亚于其术前准备工作。
0.75-0.80之间的FFR值通常被认为是灰色地带,大约有一半至少有一处病变、FFR值处于此区间的患者未进行PCI治疗。当不对这些患者纳入分析之后,FFR指导下PCI治疗和无FFR指导的患者间预后差异变得更加明显。这是一项重大的发现,它说明至少一处血流动力学显著狭窄而不进行处理时,患者结局不良。这也证实了不完全血运重建治疗会有不良影响。大而言之,这一研究也再次确立FFR值0.80为临床阈值。在FFR的初期阶段,大家普遍支持其阈值为0.75。随后将该值作为在非侵入性负荷检查中判定是否存在缺血的分水岭。即使在这些有效性研究中应用了严格的统计学方法,但仍然存在大量可逆性心脏缺血患者的FFR值高达0.80。此外,Legalery等指出在FFR值低于0.80时,行血运重建治疗往往预后不好。因此将FFR阈值提高到了0.80。Li的数据也说明0.80作为阈值是正确的。
传统意义上讲,冠心病的诊断是以冠脉造影为基础,发现至少一支心脏表面动脉有一处及多处狭窄50%以上可确诊。即使这一金标准已成明日黄花,并且对解剖和功能方面的临床决策指导意义已变得陈腐不堪,但≥50%的直径狭窄仍是判断是否进行血运重建、患者风险分层、评估非介入检查手段以及作为血运重建治疗策略研究终点的标准。对于冠脉粥样硬化和临床预后机制的理解方面,这些作者起到了不亚于"哥白尼式革命"的作用,使我们认识到,微脉管系统、心肌细胞、血小板和凝血、炎症、内皮功能不良等都在冠心病的病理生理和患者预后中起重要作用。应该认识到,我们对冠心病定义模糊是使得该病临床预后变得难以捉摸的首要原因。因此,首要目标是对冠心病进行更好的界定和治疗,目前FFR测量可对异常心外膜阻力进行精确定位与定量,将其与高质量冠脉造影相结合应用可实现对冠心病的正确诊疗,而不是应用之前的过时标准进行评价。Li的文章使我们认识到,这些新手段我们已掌握数年,使用它们可显著改善患者预后。
最终,在将FFR评估指导治疗荒废数年之后,为何我们不重拾此利器。一项回顾性注册研究对FFR指导与血管造影指导PCI治疗的远期预后进行了对比,其结论支持在临床常规应用FFR测定指导PCI治疗。
该研究发表在1月23日欧洲心脏病学杂志上,研究纳入梅奥诊所(罗切斯特,明尼苏达州)在2002到2009年间的7358例患者,将其分为有或无FFR测定指导PCI治疗两组。接受FFR测定的患者再进一步分为立即行PCI治疗和有至少一处靶血管但行延期PCI治疗两个亚组。
结果显示:相对于仅在血管造影指导行PCI治疗的患者,行FFR测定指导使得死亡和心梗发生率的降低并不显著[HR: 0.85, 95 percent CI: 0.71–1.01, P=0.06]。然而,FFR测定后行延期PCI的患者心梗发生率降低(HR: 0.46, 95 percent CI: 0.26–0.82, P=0.008)。
此外,在研究者将至少单支血管FFR值在0.75-0.80并行延期PCI的患者剔除后,他们发现FFR测定使得死亡和心梗率显著降低(HR: 0.80, 95 percent CI: 0.66–0.96, P=0.02)。之所以剔除这些患者,是因为之前有研究表明,当冠脉病变的FFR值在0.80以下时,行延期PCI治疗对患者有害
作者得出结论:行FFR测定有使患者死亡或心梗发生率降低的趋势(P=0.06),且远期预后更佳。此外,FFR指导PCI治疗使得远期预后的改善,也与之前的临床试验结论相一致,因此有力地支持了在常规治疗中使用FFR。
摘自TCTMD
与FFR相关的拓展阅读:

Long-term outcomes of fractional flow reserve-guided vs. angiography-guided percutaneous coronary intervention in contemporary practice.
Abstract
AimsFractional flow reserve (FFR) is the reference standard for the assessment of the functional significance of coronary artery stenoses, but is underutilized in daily clinical practice. We aimed to study long-term outcomes of FFR-guided percutaneous coronary intervention (PCI) in the general clinical practice.Methods and resultsIn this retrospective study, consecutive patients (n = 7358), referred for PCI at the Mayo Clinic between October 2002 and December 2009, were divided in two groups: those undergoing PCI without (PCI-only, n = 6268) or with FFR measurements (FFR-guided, n = 1090). The latter group was further classified as the FFR-Perform group (n = 369) if followed by PCI, and the FFR-Defer group (n = 721) if PCI was deferred. Clinical events were compared during a median follow-up of 50.9 months. The Kaplan-Meier fraction of major adverse cardiac events at 7 years was 57.0% in the PCI-only vs. 50.0% in the FFR-guided group (P = 0.016). Patients with FFR-guided interventions had a non-significantly lower rate of death or myocardial infarction compared with those with angiography-guided interventions [hazard ratio (HR): 0.85, 95% CI: 0.71-1.01, P = 0.06]; the FFR-guided deferred-PCI strategy was independently associated with reduced rate of myocardial infarction (HR: 0.46, 95% CI: 0.26-0.82, P = 0.008). After excluding patients with FFR of 0.75-0.80 and deferring PCI, the use of FFR was significantly associated with reduced rate of death or myocardial infarction (HR: 0.80, 95% CI: 0.66-0.96, P = 0.02).ConclusionIn the contemporary practice, an FFR-guided treatment strategy is associated with a favourable long-term outcome. The current study supports the use of the FFR for decision-making in patients undergoing cardiac catheterization.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#远期预后#
32
#PCI治疗#
24
#ART#
24
#HEART#
33