ESC2018丨CANTOS研究:卡那奴单抗作用新通路——通过IL-6抗炎降低MACE事件
2018-08-31 国际循环编辑部 国际循环
编者按:卡那奴单抗(canakinumab)为一种靶向白细胞介素-1β(IL-1β)的人源化单克隆抗体。旨在高敏C反应蛋白(hs-CRP)升高的既往有心肌梗死的患者中评估每3个月皮下注射1次卡那奴单抗对复发性心血管事件预防作用的CANTOS研究结果在去年欧洲心脏病学学会(ESC)年会首次公布。结果发现,卡那奴单抗可显著降低主要心血管不良事件(MACE)发生。
编者按:卡那奴单抗(canakinumab)为一种靶向白细胞介素-1β(IL-1β)的人源化单克隆抗体。旨在高敏C反应蛋白(hs-CRP)升高的既往有心肌梗死的患者中评估每3个月皮下注射1次卡那奴单抗对复发性心血管事件预防作用的CANTOS研究结果在去年欧洲心脏病学学会(ESC)年会首次公布。结果发现,卡那奴单抗可显著降低主要心血管不良事件(MACE)发生。
时隔1年,CANTOS研究再度携最新研究结果在2018 ESC年会上公布,分析了卡那奴单抗对IL-6信号通路的调节作用,以及对卡那奴单抗所致感染风险的理解。本文对此予以介绍,以期让广大读者了解CANTOS研究最新进展。
IL-6信号通路调节以及动脉粥样硬化事件的发生率和死亡率
哈佛医学院布莱根妇女医院Paul M Ridker教授在会上报告了CANTOS研究的这一亚组研究结果。本研究纳入CANTOS研究中的4833例受试者,最长随访时间达5年,根据治疗第3个月时所达到的IL-6治疗水平对患者进行分层(<1.65 ng/L或≥1.65 ng/L)。研究旨在探讨IL-6水平下降与心血管事件下降之间的关系;另外还探讨了基于治疗第3个月时所达到的IL-6治疗水平,接受卡那奴单抗长期治疗对MACE、心血管死亡率和全因死亡率的影响。
1、基线IL-6水平对未来心血管事件风险的影响
结果发现,基线IL-6水平较高与未来心血管事件风险增加有关。在安慰剂组中,与基线IL-6水平最低三分位数组相比,中间三分位数组以及最高三分位数组的主要终点事件即MACE的发生风险分别增加15%(95%CI:-0.14 ~ 0.54)和47%(95%CI:0.11 ~ 0.94)(趋势P值=0.007)。
次要终点(首发MACE以及因不稳定心绞痛住院需急诊血运重建治疗的复合事件,即扩展MACE)方面也获得了类似发现。与基线IL-6水平最低三分位数组相比,中间三分位数组以及最高三分位数组的扩展MACE发生风险分别增加15%(95%CI:-0.13 ~ 0.52)和40%(95%CI:0.08 ~ 0.83)(趋势P值=0.01)。图1显示了根据基线IL-6水平分层的MACE、扩展MACE、心血管死亡和全因死亡的发生率。
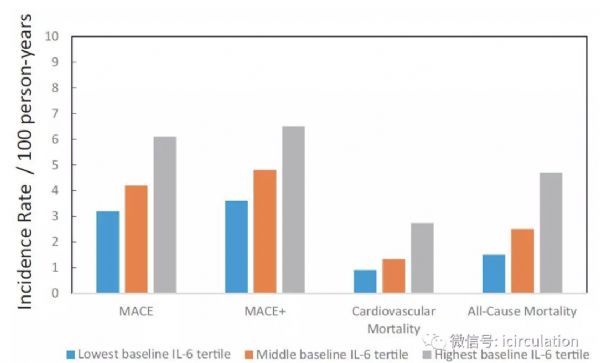
图1. 随基线IL-6水平三分位数增加,MACE、扩展MACE、心血管死亡和全因死亡的发生率
2、卡那奴单抗治疗后实现IL-6<1.65 ng/L的患者获益更大
与安慰剂组相比,第3个月时,卡那奴单抗使IL-6水平下降34.9%(P<0.001)。卡那奴单抗 50 mg、150 mg和300 mg治疗组中IL-6水平低于试验中位数值(1.65 ng/L)的患者比例分别为39%、50%和60%(P<0.0001)。与基线IL-6水平较高者相比,基线IL-6水平较低的患者在第3个月时的IL-6水平更有可能达到<1.65 ng/L。
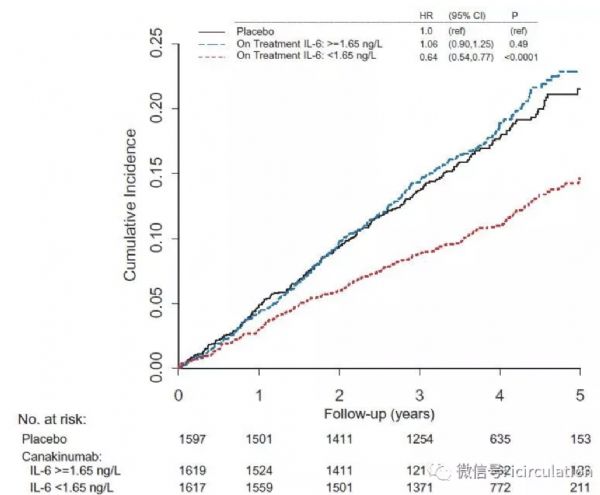
单变量分析发现,第3个月时的IL-6降幅与卡那奴单抗持续治疗的临床获益多少直接相关。具体来说,与安慰剂组相比,第3个月时,使用卡那奴单抗治疗实现IL-6<1.65 ng/L的患者,MACE下降36%(HR 0.64,95%CI:0.54 ~ 0.77;P<0.0001);而在卡那奴单抗治疗但IL-6≥1.65 ng/L的患者中未能观察到MACE下降的显著益处(图2)。而且,本研究在扩展MACE方面获得了相似发现,使用卡那奴单抗治疗在第3个月时实现IL-6<1.65 ng/L的患者,扩展MACE下降33%(HR 0.67,95%CI:0.57 ~ 0.80;P<0.0001)(图3)。另外,经过长时间治疗,接受所有剂量卡那奴单抗治疗在第3个月时实现IL-6<1.65 ng/L的患者,心血管死亡率下降57%(HR 0.43,95%CI:0.30 ~ 0.60;P<0.0001),全因死亡率下降54%(HR 0.46,95%CI:0.36 ~ 0.60;P < 0.0001)。
图2. 根据治疗3个月时IL-6≥1.65 ng/L或<1.65 ng/L,
安慰剂组和卡那奴单抗组的MACE累积发生率
图3. 根据治疗3个月时IL-6≥1.65 ng/L或<1.65 ng/L,
安慰剂组和卡那奴单抗组的扩展MACE累积发生率
总结来看,在本亚组研究中,卡那奴单抗治疗后的IL-6降幅与预期卡那奴单抗长期治疗的临床获益密切相关。CANTOS研究表明,用卡那奴单抗靶向IL-1β到IL-6的先天免疫途径可以降低心血管事件发生率。因此,CANTOS提供了关键的概念验证,即在没有降脂或降低血压的情况下,抑制炎症可以改善动脉粥样硬化性血栓结局。目前的分析结果也支持以下假设,即IL-6抑制至少在一定程度上是CANTOS中观察到事件减少的一种机制。这些数据提示今后可开展更多工作,观察靶向IL-6抑制是否也可以成为治疗动脉粥样硬化的一种有效抗细胞因子策略。
理解卡那奴单抗治疗的感染风险
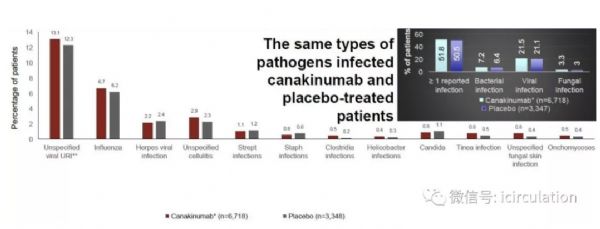
CANTOS研究结果表明,卡那奴单抗显著减少MACE发生率,但可小幅增加致死性感染风险。为了解减少感染的措施,哈佛医学院布莱根妇女医院Peter Libby教授等人对CANTOS数据进行了分析并在本届ESC年会上做了相关报告。结果发现,卡那奴单抗治疗患者发生感染的危险因素包括年龄和慢性肾脏疾病。研究期间,最常报告的严重感染包括败血症、蜂窝织炎及肺炎(图4)。但是,卡那奴单抗治疗不会额外增加机会性感染或结核病的发生风险。结果提示,某些患者特征有助于提高我们对卡那奴单抗治疗所致感染风险的意识,并对疑似细菌感染者考虑进行早期抗菌治疗。另外,CANTOS研究发现的癌症死亡率显著下降,在很大程度上平衡了卡那奴单抗治疗相关感染所致的死亡增加。
图4. CANTOS研究中常报告的感染
小结
从本届ESC年会上展示的CANTOS研究最新结果可见,卡那奴单抗治疗后的IL-6降幅与预期卡那奴单抗长期治疗的临床获益密切相关,表明用卡那奴单抗靶向IL-1β到IL-6的先天免疫途径可以降低心血管事件发生率。在安全性方面,某些患者特征有助于提高我们对卡那奴单抗治疗所致感染风险的意识,并对疑似细菌感染考虑进行早期抗菌治疗。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#ACE#
0
#MAC#
40
#ESC2018#
36
#卡那奴单抗#
41
#IL-6#
45
#MACE#
33
了解一下,谢谢分享!
82