2016世界艾滋病日:全景科普
2016-12-01 《中国病毒学(英文版)》编辑部” 《中国病毒学(英文版)》编辑部”
2016年12月1日迎来了全球第29个“世界艾滋病日”。今年的活动主题依旧为:行动起来,向‘零’迈进(英文主题为Getting to Zero)。 艾滋病自1981年被发现至今30余年,肆虐全球,夺去了3500多万人的生命,发展成为一个严重的全球范围的公共卫生和社会问题。艾滋病到底是一种什么样的病?有什么有效的治疗措施,又该如何防控? 1.什么是艾滋病? 艾滋病是获得
2016年12月1日迎来了全球第29个“世界艾滋病日”。今年的活动主题依旧为:行动起来,向‘零’迈进(英文主题为Getting to Zero)。

图1 全球HIV感染分布。Sources: UNAIDS2016 estimates 全球2015年新发HIV感染者210万,包括15万左右的儿童。其中非洲东部和南部感染人数约为96万,约占总感染人数的45.7%,非洲西部和中部HIV感染者人数约为41万,亚太地区为30万,新发感染区域分布与全球HIV感染者区域分布比例类似。

图2 全球2015年新增HIV感染者(按地区分布)。Sources: UNAIDS2016 estimates 据世界卫生组织(WHO)最新的统计分析,艾滋病肆虐全球,已夺去了3500多万人的生命,仅2015年就有110万人死于艾滋病,图2中为全球每年(包含了所有年龄段)死于艾滋病的人数统计,从UNAIDS统计数据中可以看出随着对艾滋病的科学理解、预防和治疗的逐步完善、世界卫生组织和各国政府以及人民的积极努力下,艾滋病的死亡人数呈下降趋势,有力的说明了艾滋病毒可以有效的控制,有效的治疗可以改善HIV患者的生存状态。
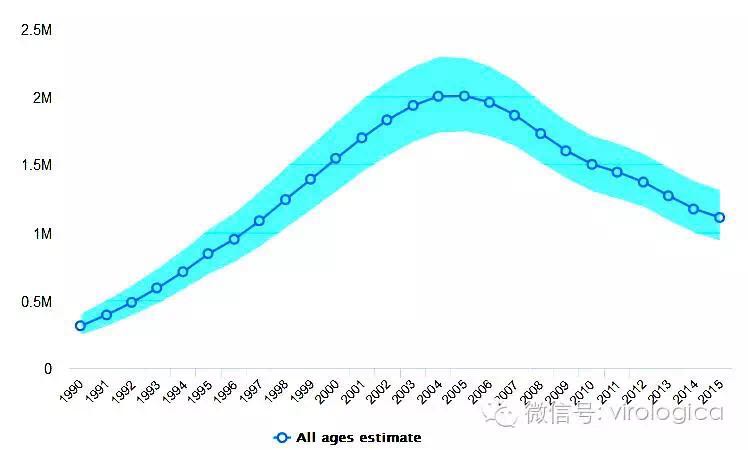
图3 全球每年死于艾滋病的人数统计。Sources: UNAIDS2016 estimates 据国家卫生计生委疾病预防控制局统计,我国艾滋病感染人数呈现增长趋势,其中2015年全国艾滋病发病50330例,死亡12755人,发病率为3.6940/10万,死亡率为0.9362/10万。 2.HIV为何能肆虐全球? HIV病毒,一种攻击人类免疫系统的慢病毒(Lentivirus),属逆转录病毒的一种,艾滋病毒直径约120纳米,呈球形,由类脂包膜、包膜蛋白、衣壳组成。衣壳内含有含有病毒的RNA基因组、酶(逆转录酶、整合酶、蛋白酶)以及其他来自宿主细胞的成分。目前已知的艾滋病病毒共有4种,分别是M、N、O、P,均来自喀麦隆的黑猩猩及大猩猩,其中源自黑猩猩的M和N传播最广,其他两种源于大猩猩的病例较少,O型只有10万人,而P型仅2例。
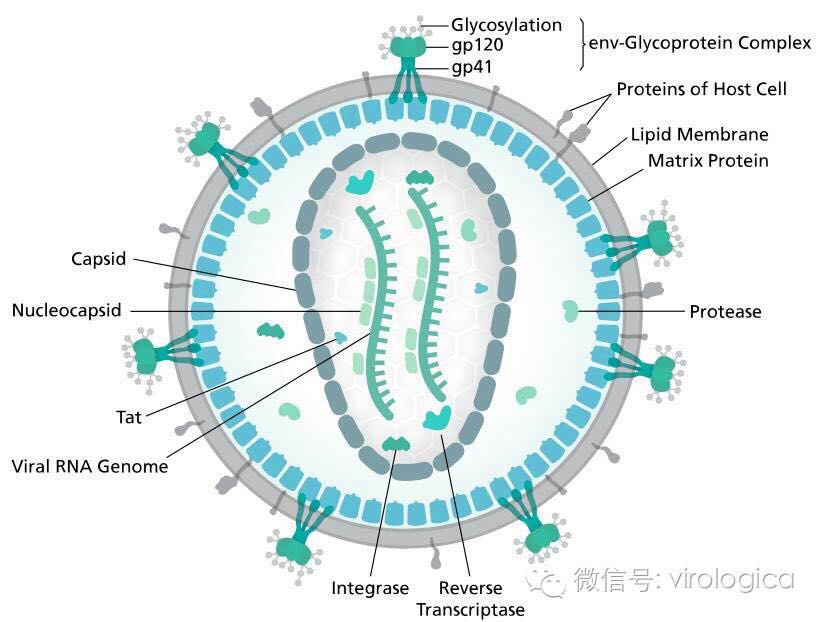
图4 HIV病毒结构示意图 人体的免疫系统由淋巴结、胸腺、脾脏、骨髓和淋巴细胞(主要为T、B淋巴细胞)所组成,人体的免疫系统有多种途径消灭入侵者,当人体感染病毒时,首先淋巴系统的巨噬细胞吞噬病毒,并将抗原信息提呈在细胞表面并传递给TH细胞(CD4 T细胞),进一步传递产生抗体将病毒清除。 HIV病毒因直接感染CD4 T细胞而阻断了人体的免疫应答,一旦受感染的CD4 T细胞活化,随着CD4 T细胞的复制和繁殖,病毒也随着完成了复制和繁殖,当大量的HIV病毒从CD4 T细胞“破壁而出”时,细胞本身也就凋亡了。 3.艾滋病的传播途径 过去:20世纪90年代,在我国,血源性传播是HIV传播的主要途径,其中包括静脉注射吸毒、血液和血液制品以及不洁医疗器械传播。 现在:性传播成为艾滋病流行的新特点,高危人群主要是同性恋或异性恋、暗娼和外来务工人员,其中异性性传播是HIV病毒性传播的主要因素。 其他传播方式:母婴垂直传播——母婴垂直传播发生在孕期、分娩时和产后哺乳期,母体内病毒载量越高,围产期母婴传播的危险性就越大。 4.人类感染艾滋病的症状 人类感染HIV后,根据多数感染者呈现的症状,主要划分为三个阶段: <1>急性期 人体感染HIV后2-4周,多数感染者会出现类似感冒的症状如发热、咽痛、头疼、皮疹等急性感染症状。该阶段HIV病毒利用CD4T细胞大量繁殖,因此体内CD4T细胞水平急剧下降,随后人体免疫应答将会使得HIV病毒处于一个相对稳定的水平(viral set point),此时的T细胞会慢慢增多,但很难达到感染前的水平。 <2>无症状期 急性期过后,人体会进入一个无症状期(clinical latency stage),临床上没有任何症状,但血清中能检出HIV及HIV核心蛋白和包膜蛋白的抗体,具有传染性。本期时间长短因每个个体病程进展而不同,持续时间一般为6-8年。 <3>艾滋病期 该期为感染HIV最终阶段。人体免疫系统被严重破坏,当体内CD4T细胞数目下降到<200个/mm3时,就认为进入艾滋病期,此期的主要临床表现为HIV相关症状、各种机会性感染及肿瘤。

图5 HIV感染进程(未接受治疗) 5.如何确诊是否感染HIV病毒 依靠上述症状并不能确定一个人是否感染HIV病毒,唯一的确诊方法是接受检测, HIV感染有哪些检测指标呢? 大多数感染者在初次感染3到12周会产生特异性抗体(这一时期称为血清转化),血清转化前的HIV感染者主要检测HIV-RNA或者是HIV衣壳蛋白P24抗原,检测结果阳性者通过抗体检测或PCR来确诊。其中小于18个月的婴儿因体内尚存母源抗体而不能采用抗体检测,只能通过P24抗原检测及PCR扩增HIV RNA或者DNA及的手段来确诊。 6.艾滋病的治疗 临床采用组合药物治疗艾滋病的感染,这种疗法称为抗逆转录病毒疗法(ART),该疗法适用于所有艾滋病感染者,其原理就是利用抗艾药物组合,阻断艾滋病在体内的扩增,为免疫系统的恢复提供机会。尽管该方法并不能治愈艾滋,但通过控制HIV病毒数量,强大免疫系统,可以强有力的对抗各种机会感染和肿瘤,同时降低HIV病毒传播的机会。 图6中显示,从2000年起,全球HIV感染者接受ART治疗的人数每3到4年就会翻一番。在2000年只有69万人接受了ART治疗(2000年总HIV感染者约286万),。到2014年,在约369万HIV中,有149万正接受ART治疗,统计结果显示至2014年ART治疗覆盖率从2000年的2%上升到到40%。同时从图5艾滋死亡人数统计结果来看,随着ART治疗的覆盖的扩大,HIV感染者的生存环境得到很大的改善,艾滋病死亡人数呈现出下降趋势。
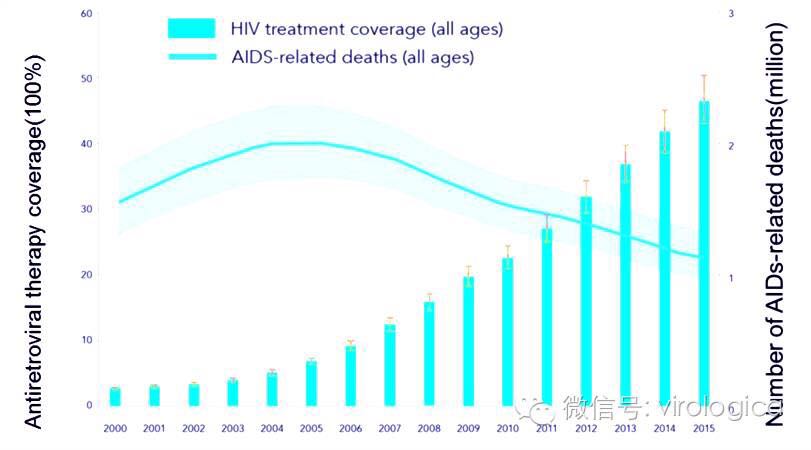
图6 HIV ART治疗覆盖率及全球艾滋死亡人数统计(2000年—2015年) 临床上治疗艾滋病的药物分为6类: <1>非核苷类逆转录酶抑制剂(NNRTIs) <2>核苷类逆转录酶抑制剂(NRTIs) <3>蛋白酶抑制剂(PIs) <4>融合抑制剂(Fusion inhibitors) <5>CCR5拮抗剂(CCR5s) <6>整合酶链转移抑制剂(INSTIs) 其中NNRTIs和NRTIs通过结合并抑制HIV逆转录酶活性,抑制HIV的逆转录过程,从而阻断病毒的复制。PIs通过抑制蛋白酶的活性从而阻断HIV病毒的包装成熟,使其无法侵袭其他CD4T细胞。融合抑制剂能通过阻止HIV病毒包膜对CD4T细胞的附和从而阻止病毒的入侵。CCR5s能够与HIV病毒结合竞争结合CD4T细胞的CCR5辅助受体,从而抑制HIV病毒对CD4T细胞的入侵,INSTIs则通过抑制HIV整合酶的活性,从而抑制其DNA整合到宿主DNA上,达到抑制其DNA的复制的目的。 目前HIV药物治疗的局限 HIV病毒不能治愈的原因有以下几点: 病毒复制速度相当快。 HIV病毒边复制边变异,即使是采用目前较先进的“鸡尾酒疗法”很长时间后,感染者体内病毒载量依然很高。 HIV病毒DNA整合到CD4+T细胞DNA,当有其他病毒感染时会随之复制。所以要清除体内病毒相当有难度。 实际中,抗病毒药物还有很多副作用,如短期的副作用可能会出现贫血、腹泻、头晕、乏力、恶心、焦虑、皮疹,长期的副作用还包括脂肪代谢障碍、胰岛素耐受、血脂异常、乳酸血症等,感染者可能会出现不听从医嘱而间断服药,给病毒繁殖和变异留下空间。 7.艾滋病的预防 虽然目前艾滋病还没有特效治疗药物,但是艾滋病得流行史表明,艾滋病是一种完全可以预防的疾病。 性接触:使用避孕套可以将感染HIV病毒的风险降低80%。 艾滋病暴露前预防(Pre-exposur):通过抗逆转录病毒药物治疗,控制CD4T细胞中HIV数目≤ 550个/ul是一种非常有效的防治艾滋病毒传染给性伴侣的方法。 艾滋病暴露后预防(Post-exposure):在接触HIV阳性血液或者是生殖器分泌物后的48至72小时,该阶段成为暴露后预防,采用抗逆转录病毒药物治疗能有效降低HIV感染的风险。 垂直传播预防(Mother-to-child):采取奶瓶喂奶,同时在孕期及产后采用抗逆转录病毒药物治疗来预防HIV垂直传播,可以将感染风险减少92–99%。 接种疫苗:目前还没有HIV/AIDs的临床许可疫苗,迄今研究发现的最为有效的疫苗,2009年公布的RV144,可降低部分HIV感染者约30%的传染率,这个消息足以振奋人心,RV144的进一步研究仍在继续。 控制艾滋病的流行,更为重要的是各个国家出台高效的防艾政策,采取严格有效的预防措施,唤起大众人群对艾滋病人的同情和理解,给HIV感染者更多的关怀,人类就一定能将艾滋病带来的危害降到最低,战胜艾滋病的目标终会实现。 (本文由中南大学康怀兴博士供稿) 原始出处:
1.Alimonti J B, Ball T B, Fowke K R. Mechanisms of CD4+ T lymphocyte cell death in human immunodeficiency virus infection and AIDS[J]. Journal of general Virology, 2003, 84(7): 1649-1661. 2. Zhang C, Zhou S, Groppelli E, et al. Hybrid spreading mechanisms and T cell activation shape the dynamics of HIV-1 infection[J]. PLoS Comput Biol, 2015, 11(4): e1004179. 3. Hel Z, McGhee J R, Mestecky J. HIV infection: first battle decides the war[J]. Trends in immunology, 2006, 27(6): 274-281. 4. World Health Organization. WHO case definitions of HIV for surveillance and revised clinical staging and immunological classification of HIV-related disease in adults and children[J]. 2007. 5. Lo C W, Wu K G, Lin M C, et al. Application of a molecular method for the classification of human enteroviruses and its correlation with clinical manifestations[J]. Journal of Microbiology, Immunology and Infection, 2010, 43(5): 354-359. 6. Crosby R, Bounse S. Condom effectiveness: where are we now?[J]. Sexual health, 2012, 9(1): 10-17. 7. Anglemyer A, Rutherford G W, Baggaley R C, et al. Antiretroviral therapy for prevention of HIV transmission in HIV‐discordant couples[J]. The Cochrane Library, 2011. 8. [No authors listed]. HIV exposure through contact with body fluids.[J]. Prescrire International, 2012, 21(126). 9. Kurth A E, Celum C, Baeten J M, et al. Combination HIV Prevention: Significance, Challenges, and Opportunities[J]. Current HIV/AIDS Reports, 2011, 8(1):62-72. 10. Girard M P. [The quest for an HIV vaccine].[J]. Bulletin De Lacadémie Nationale De Médecine, 2005, 189(5). 11. World Health Organization [WHO]. Department of HIV / AIDS. Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV Infection: Recommendations for a Public Health Approach.[J]. Geneva Switzerland Who, 2013. 12. World Health Organization [WHO]. Department of HIV / AIDS. Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV Infection: Recommendations for a Public Health Approach.[J]. Geneva Switzerland Who, 2013. 13. Brown T T, Qaqish R B. Antiretroviral therapy and the prevalence of osteopenia and osteoporosis: a meta-analytic review.[J]. Aids, 2006, 20(17):2165-74. 14. Cohen M S, Hellmann N, Levy J A, et al. The spread, treatment, and prevention of HIV-1: evolution of a global pandemic.[J]. Journal of Clinical Investigation, 2008, 118(4):1244-54. 15. Sharp P M, Hahn B H. Origins of HIV and the AIDS pandemic[J]. Cold Spring Harbor Perspectives in Medicine, 2011, 1(1):1639-1647.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#全景#
26
#世界艾滋病日#
35
小编辛苦了!为我们整理如此齐全的资料,供学习探究。点赞啦!谢谢!
50
真的很有必要
53
让大家看到这篇文章
59
66
43