ACC 2018:鼓舞人心!ODYSSEY OUTCOMES研究新鲜出炉
2018-03-10 郭远林 中国医学论坛报今日循环
3月10日-12日,第67届美国心脏病学年会(ACC2018)在美国奥兰多盛大召开。当地时间3月10日上午,ODYSSEY OUTCOMES研究正式发布。
3月10日-12日,第67届美国心脏病学年会(ACC2018)在美国奥兰多盛大召开。当地时间3月10日上午,ODYSSEY OUTCOMES研究正式发布。
ODYSSEY OUTCOMES研究堪称2018ACC年会“最新临床试验”专场最为专家学者们关注的一项研究。
ODYSSEY OUTCOMES研究共纳入18,924例经强化他汀治疗LDL-C仍高于70mg/dL的ACS患者,在维持现有最佳治疗的基础上随机分为两组:PCSK9全人单克隆抗体Alirocumab干预组或安慰剂组。
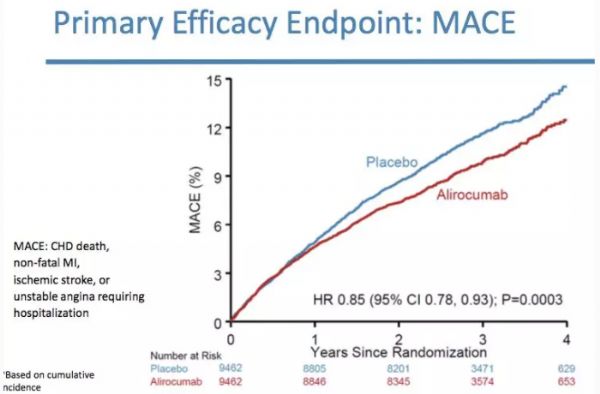
经过中位随访时间为2.8年的治疗,ODYSSEY OUTCOMES研究终于证实了其科学设想,今天公布了其鼓舞人心的结果:Alirocumab组不仅心血管主要终点事件显著降低15%,且全因死亡风险降低15%(在这一点上甚至超出预期);与此同时,除了注射部位局部反应之外,没有出现包括新发糖尿病、认知障碍、出血性卒中、白内障等在内的任何安全性问题(图)。
图 研究主要结果
01 研究设计独一无二
ODYSSEY OUTCOMES研究设计的独特、超前主要体现在随机后Alirocumab的干预模式是围绕治疗后LDL-C水平的滴定式干预而不是固定剂量(75mg Q2W或150mg Q2W或过低停用,且每次剂量调整均采用双模拟模式以确保双盲)。
这是20余年来降脂干预与心血管硬终点临床试验中的第一项也是目前唯一一项根据LDL-C水平滴定降脂药物剂量的研究。
该研究设计体现了本着LDL-C原则的降脂治疗模式,且符合真实世界的实践与操作,将成为血脂指南进一步更新与完善的重要依据,尤其是在目标值设定方面,乃是填补空白。
更为创新的是,研究设计的剂量滴定模式不仅有LDL-C目标值上限、同时设定了其下限,即探索的是一个明确的LDL-C目标范围(目标25mg/dL-50mg/dL,允许15mg/dL-25mg/dL,低限15mg/dL)的获益与安全性,旨在为临床实践中争议颇多的LDL-C低限问题提供循证医学证据。
02 研究结果填补空白
低水平LDL-C的安全性
尽管去年ACC年会公布的FOURIER研究已证实PCSK9单抗Evolocumab能在他汀基础上进一步改善心血管风险转归,且低水平LDL-C的安全性良好。
但该研究因Evolocumab组获益明显而提前结束、中位随访时间仅2.2年,给长期应用的安全性问题留下了疑问。
而ODYSSEY OUTCOMES研究的中位随访时间为2.8年,其中44%的患者随访时间超过3年,接近既往降脂干预RCT研究的随访时间,填补了较长期应用PCSK9单抗安全性证据的空白,一定程度上回答了PCSK9单抗长期应用及其带来的低水平LDL-C的安全性问题。
降低全因死亡风险
ODYSSEY OUTCOMES研究结果首次证实PCSK9单抗Alirocumab使全因死亡风险降低15%(绝对风险降低0.6%),P=0.026。
进一步分析显示,随机时基线LDL-C>100mg/dL的亚组其全因死亡风险获益尤为显著(相对风险降低29%;绝对风险降低1.7%)。
这不仅是PCSK9单抗首次证实对全因死亡的获益,也填补了强化降LDL-C治疗对全因死亡风险获益证据上的空缺。
设定LDL-C目标值的证据
2013年美国ACC/AHA降胆固醇治疗指南提出取消LDL-C目标值,理由是既往他汀RCT研究均不是基于为达到预设LDL-C目标值而进行的研究、因而缺乏设定LDL-C目标值的直接证据。
ODYSSEY OUTCOMES研究则首次证实了以LDL-C达标与否为导向的剂量滴定调脂模式下的心血管获益,不仅填补了这方面证据的空白,更是“胆固醇理论”、“LDL-C定律”的又一力证,对指南及实践意义重大。
遗憾的是中国包括台湾在内一共仅700余例参与该研究。此外,低水平LDL-C安全性的问题仍然有待更长时间的观察与随访。期待后续关于ODYSSEY OUTCOMES研究的详细数据及进一步分析,以便更全面科学地解读这一里程碑式的循证医学证据以指导临床实践、造福患者。
原始出处:
Presented by Dr. Philippe Steg. Evaluation of Cardiovascular Outcomes After an Acute Coronary Syndrome During Treatment With Alirocumab - ODYSSEY OUTCOMES. American College of Cardiology Annual Scientific Session (ACC 2018), Orlando, FL, March 10, 2018.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







学习了.谢谢分享
77
学习了谢谢分享!!
75
#ACC#
36
#MES#
36
学习了
81
学习一下谢谢
60
除了贵目前看来是未来最有可能取代他汀的调脂药物
59
学习了.谢谢分享
26
作为一项最早设计的旨在证实PCSK9单抗Alirocumab能在他汀基础上对心血管硬终点进一步带来获益的大规模国际多中心临床试验.其研究结果确实众目所盼.
31