患者男性,42岁,既往患有糖尿病,近日因出现严重排尿困难和尿失禁几天余而到急诊科就诊。
实验室检查结果显示脓尿,白细胞增多(白细胞计数为10820/mm3)、C-反应蛋白水平升高(134.1mg/L),高血糖(血糖水平900mg/dL)以及糖化血红蛋白水平升高(11.4%)。
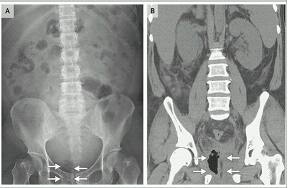
肾、输尿管造影检查显示耻骨联合右侧膀胱内部可见非典型的焦点(图A,箭头)。
随后行腹部计算机断层扫描(CT)显示气肿性前列腺炎(图B,箭头)。
随即,会诊医师根据该患者的情况,对其进行留置导尿管,并在CT引导下经皮穿刺引流前列腺分泌液。
同时,应用广谱抗生素和静脉补液治疗,并实施了严格的血糖控制与胰岛素滴注。
此外,尿液和血液培养中都发现了肺炎克雷伯菌的存在。
最后,该患者因感染、败血症和高血糖以及急性肾损伤住院治疗1个月。随后,病情逐渐好转,顺利康复出院。
气肿性前列腺炎是一种罕见的尿路感染并发症,最常见于免疫抑制、糖尿病血糖控制不良、肝硬化、酒精中毒,或最近行尿道手术的患者。
在本案例中,患者是一名糖尿病患者,在这种情况下,最常见的发病病原体是肺炎克雷伯菌。
原始出处:
Hsun-Shuan Wang, M.D.Ming-Chen Shih, M.D. Emphysematous Prostatitis
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












很好,不错,以后会多学习
58
很好,不错,以后会多学习
58
很好,不错,以后会多学习
54
继续学习
66
继续关注
60