Chest:无创间歇正压通气在重度脊柱侧凸运动中的作用
2021-09-17 从医路漫漫 MedSci原创
无创间歇正压通气(NIPPV)可改善COPD患者的运动表现。目前尚不清楚这是否也适用于其他患者群体,如限制性呼吸系统疾病患者。
研究目的:无创间歇正压通气(NIPPV)可改善COPD患者的运动表现。目前尚不清楚这是否也适用于其他患者群体,如限制性呼吸系统疾病患者。
设计:进行一项随机对照试验,有8例严重先天性脊柱侧凸患者参与研究。
干预:通过接口器施加NIPPV,进行次极量平板运动试验。每位受试者随机进行三次行走,使用三个不同的呼吸机呼吸,一次步行通过接口器呼吸,按随机顺序进行。此外,还进行了四次正常无负重的行走呼吸,无需监测。
测量和结果:四次正常无负重的行走没有显示出显着的学习效果。平均步行距离为204米(134.9米)。单独使用接口器,步行距离下降到140米(75.8米),加上呼吸机,步行距离进一步下降到109米(59.3米)。分组效应方差分析显示,不同的步行方式在步行距离上有显著差异(p=0.048)。三种品牌的呼吸机没有差异。在运动的节点,呼吸机辅助步行的潮气量和小潮气量(Mv)与单独使用接口器的步行相比显着增加(p<0.05)。
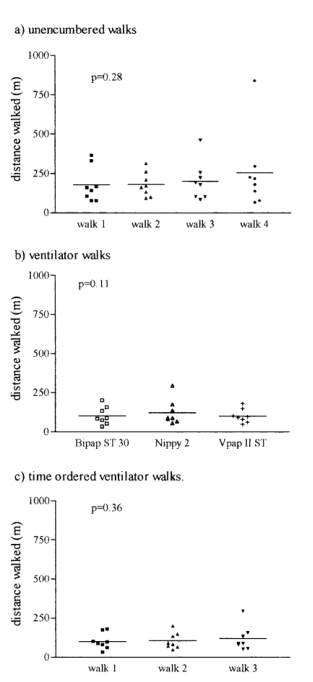
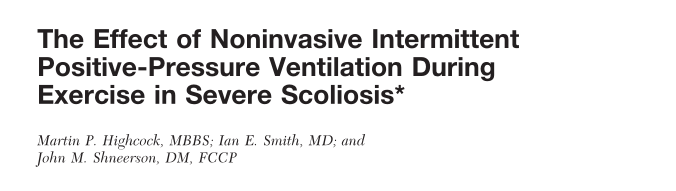
图1 显示步行距离,与个别数据点和组的平均值。p值使用重复测量的方差分析进行计算。
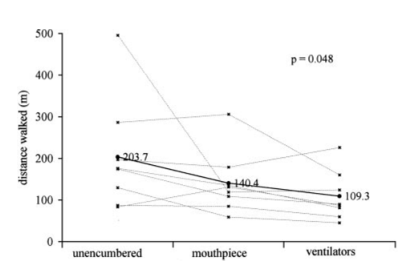
图2 根据类型、单个数据点和分组平均值显示步行距离。采用混合效应方差分析和按类型比较步行的方法计算p值。
表1 步行运动后的结果
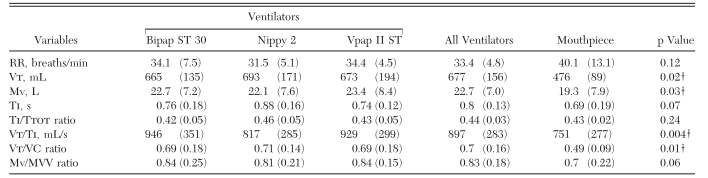
表2 运动节点处的数据
结论:尽管观察到Mv增加,但通过接口器呼吸会减弱运动耐力,并且使用呼吸机呼吸也没有改善。NIPPV对严重脊柱侧凸弯患者的运动耐力无有益作用。
原文出处
Highcock MP, Smith IE, Shneerson JM,The effect of noninvasive intermittent positive-pressure ventilation during exercise in severe scoliosis.Chest 2002 May;121(5)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#EST#
28
#Chest#
44
#脊柱侧凸#
30
#正压通气#
34
厉害
45