Neurology: 25年随访研究发现心脏结构和功能与中年时认知有关
2022-03-16 影像小生 MedSci原创
该研究结果提供了将早期至中年心脏结构和功能与认知联系起来的信息。
已有研究发现心脏结构、收缩功能、舒张功能的亚临床异常与低认知能力之间存在联系,特别是在老年人中;然而,研究结果存在矛盾。不一致性可以通过选择患有终末期心脏病的研究人群来解释。此外,尚不清楚青年期心脏结构和功能的亚临床异常是否会影响大脑健康。这些异常很常见,而且大多未得到充分诊断;因此,心脏结构和功能的改变是否可能是认知障碍的一个风险因素的问题具有重大的公共健康影响,并可能揭示另一个重要的心脑联系。
Laure Rouch等在Neurology杂志发表题为Twenty-Five-Year Change in Cardiac Structure and Function and Midlife Cognition: The CARDIA Study的研究文章,确定中年心脏结构和功能及其从成年早期到中期的 25 年变化是否与中年认知能力下降有关。

该实验研究了来自年轻人冠状动脉风险发展 (CARDIA) 研究的 2653 名参与者(57% 为女性,46% 为黑人)。在第 5、25 和 30 年(参与者平均年龄 30、50 和 55 岁)时获得超声心动图,以评估左心室 (LV) 质量 (LVM)、LV 收缩功能与 LV 射血分数 (LVEF) 和 LV 舒张压功能与左心房容积 (LAV) 和早期峰值二尖瓣速度 (E)/早期峰值二尖瓣环速度 (e') 比率。LVM 和 LAV 以体表面积(LVMi 和 LAVi)为指标。在 30 年时,测量了 5 个认知领域:整体认知、处理速度、执行功能、延迟的语言记忆和语言流利度。使用线性回归调查了中年(30 年)和 25 年心脏结构和功能变化对中年认知的影响。
25 年来,LVMi 和 LAVi 每年平均变化 (SD) 分别增加 0.27 (0.28) g/m 2和 0.42 (0.15) mL/m 2,而 LVEF 下降了 0.11% (0.02%)。
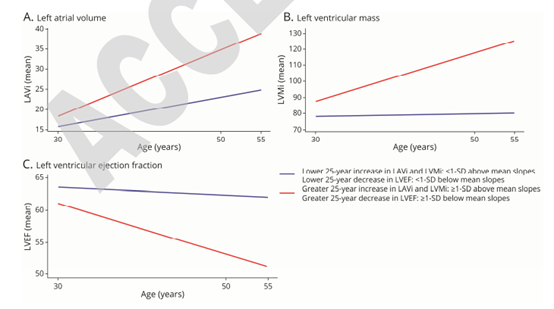
超声心动图参数(斜率)25年的变化
调整人口统计和教育水平后,25 年LVMi 增加(≥1 SD)与大多数测试的认知能力降低有关(p ≤ 0.02);
25 年 LAVi 增加与较低的整体认知相关 ( p = 0.04),
但 25 年LVEF 减少与认知无关。

25年心脏结构和功能的改变和中年认知
对心血管危险因素的进一步调整得到了类似的结果。
此外,与 30 年时 E/e' 比率和 LVEF 不同,较高的 30 年 LVMi 和 LAVi 与大多数认知测试中的较差认知显著相关。
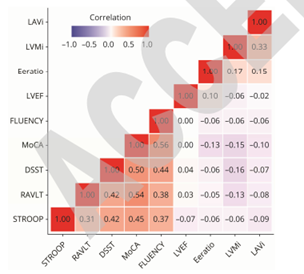
中年心脏结构和功能与中年认知热图
即使在考虑了混杂因素之后,中年心脏结构及其从成年早期到中期的变化也与较低的中年认知有关。与收缩功能不同,中年左室舒张功能及其 25 年的变化也与认知有关。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#研究发现#
55
#随访研究#
57
#Neurol#
38
#心脏结构#
60
#5年随访#
63